QT Prolongation Risk Estimator
Estimate Your Risk
When you’re managing a serious mental health condition like schizophrenia, the last thing you want to worry about is your heart. But for many people taking antipsychotic medications, that’s exactly the risk they face-especially when those drugs are combined with heart medications. The issue isn’t just theoretical. It’s called QT prolongation, and it can turn a routine prescription into a life-threatening situation.
What Is QT Prolongation?
The QT interval on an ECG measures how long it takes your heart’s ventricles to recharge between beats. If that interval stretches too long, your heart can develop a dangerous rhythm called torsade de pointes. This isn’t just an abnormal ECG reading-it can lead to fainting, seizures, or sudden cardiac death. The corrected QT interval, or QTc, adjusts for heart rate. A QTc over 500 milliseconds is considered high risk. An increase of more than 60 ms from your baseline is also a red flag.Why Antipsychotics Are a Problem
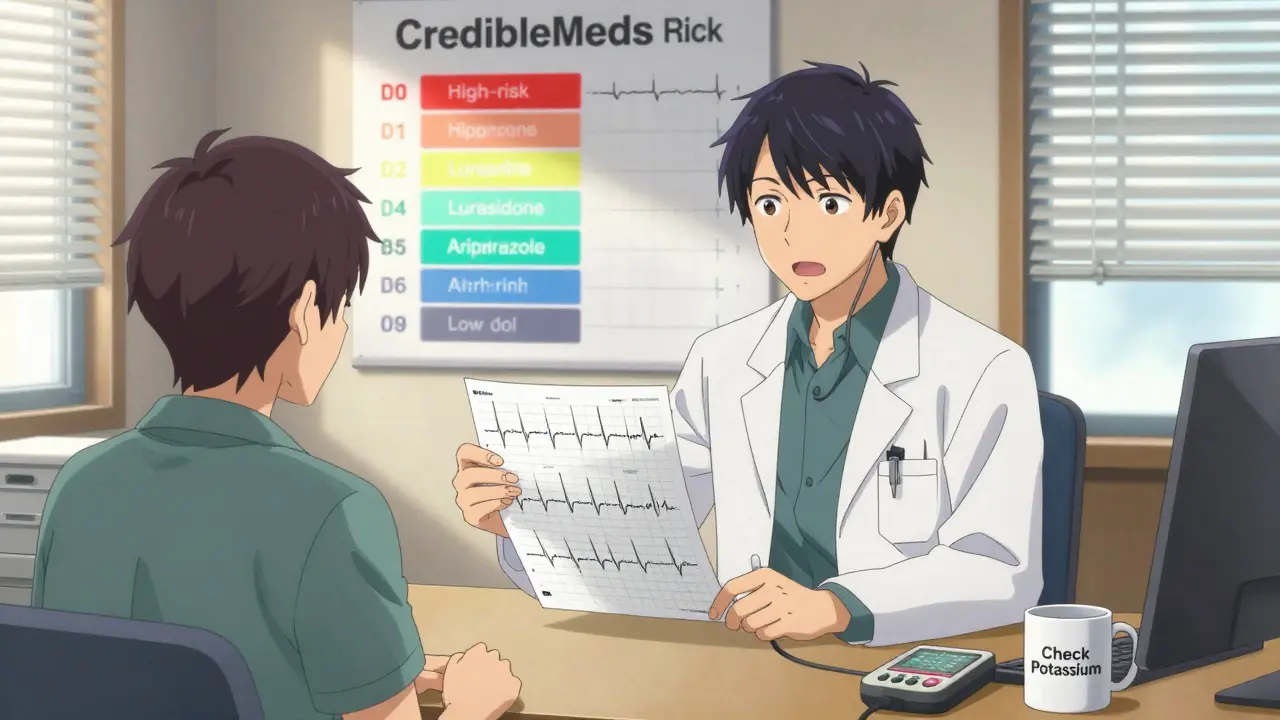
Almost all antipsychotic drugs affect the heart’s electrical system. Some more than others. Thioridazine, pulled from the U.S. market in 2005, could stretch the QT interval by up to 35 milliseconds. That’s massive. Haloperidol and olanzapine? They add about 4 to 6 ms. Lurasidone? Barely any effect at all. The risk isn’t random. It’s ranked. CredibleMeds, a trusted drug safety database, classifies antipsychotics into three tiers:- High risk: Thioridazine (no longer sold), haloperidol, ziprasidone
- Moderate risk: Risperidone, quetiapine, iloperidone
- Low risk: Aripiprazole, brexpiprazole, lurasidone, paliperidone
Even if you’ve never heard of ziprasidone, you should know this: it’s been flagged by the FDA with a black box warning for QT prolongation. But here’s the twist-a 2023 study in JAMA Network Open found no significant QT increase in ICU patients given ziprasidone or haloperidol, as long as their baseline QTc was under 550 ms. So context matters. A healthy person on a single drug is very different from an older patient on five medications with low potassium.
Cardiac Medications Make It Worse
It’s not just antipsychotics. Many heart drugs also prolong QT. Think:- Antiarrhythmics like amiodarone and sotalol
- Antibiotics like moxifloxacin
- Antifungals like fluconazole
- Some antidepressants, including citalopram and escitalopram
When you stack these on top of antipsychotics, the risk multiplies. A study at Toulouse University Hospital found that 68% of patients with QTc over 500 ms were taking two or more QT-prolonging drugs. That’s not coincidence-it’s a pattern. The British Heart Rhythm Society calls this polypharmacy danger zone. And it’s why so many clinicians now check for drug interactions before prescribing.
Who’s Most at Risk?
Not everyone who takes these drugs will have problems. But some people are far more vulnerable:- Women: 1.7 times more likely than men to develop QT prolongation
- People over 65: 2.3 times higher risk
- Low potassium or magnesium: Hypokalemia (potassium below 3.5 mmol/L) was found in 28% of cases with prolonged QT
- Heart disease: History of heart failure, prior arrhythmias, or long QT syndrome
- Genetics: Some people inherit a predisposition to QT prolongation
These aren’t just statistics. They’re real people. A 72-year-old woman with schizophrenia, on haloperidol, with mild kidney disease and low potassium, is in a danger zone. Her doctor needs to know that.
What Should Doctors Do?
Guidelines are clear. The British Heart Rhythm Society and the Maudsley Prescribing Guidelines say:- Get a baseline ECG before starting any antipsychotic-especially high-risk ones.
- Repeat the ECG within one week after reaching a steady dose.
- Check electrolytes. Keep potassium above 4.0 mmol/L and magnesium above 1.8 mg/dL.
- Review all medications. Remove or replace any other QT-prolonging drugs if possible.
- For high-risk patients, consider continuous cardiac monitoring in hospital.
- Monitor annually, even if you’ve been stable for years.
But here’s the problem: only 73% of psychiatrists routinely order baseline ECGs for high-risk antipsychotics. Only 32% do it for moderate-risk drugs. And 68% of non-cardiologists misread QT intervals without special training. That’s not just a gap-it’s a hazard.
What Happens When QT Prolongation Is Found?
If your QTc jumps over 500 ms or increases by more than 60 ms from baseline, action is needed. Most cases are reversible:- 62% of patients improved with a dose reduction
- 28% got better after switching to a lower-risk antipsychotic (like lurasidone or aripiprazole)
- 57% saw correction after fixing electrolyte imbalances
Stopping the drug entirely is rare-and often unnecessary. The real danger isn’t the medication. It’s avoiding it. People with schizophrenia who don’t take antipsychotics have a 5% lifetime suicide risk and a 12% higher chance of accidental death. Studies show they’re 40% more likely to die early than those who take them. The goal isn’t to avoid antipsychotics. It’s to use them safely.
The Bigger Picture: Risk vs. Benefit
There’s a U-shaped curve when it comes to mortality. People who take no antipsychotics die early. People on very high doses die early. But those on low-to-medium doses? They live longer. That’s because the drugs control psychosis, reduce aggression, prevent suicide, and improve adherence to physical health care.Dr. David M. Taylor, who wrote the Maudsley Guidelines, says it plainly: “Assume all antipsychotics carry an increased risk of sudden cardiac death. But antipsychotics can protect patients against the consequences of schizophrenia.”
That’s the tightrope. You can’t ignore the heart. But you can’t ignore the mind either.
What’s Changing Now?
The FDA now requires every new antipsychotic to undergo a thorough QT (TQT) study with over 100 healthy volunteers. That’s why newer drugs like lurasidone and lumateperone have such clean safety profiles. Sales of low-risk antipsychotics rose 14.2% in 2022. Haloperidol sales dropped 3.7%. Hospitals are updating formularies. Sixty-three percent of U.S. academic medical centers now have QT risk-based prescribing rules.By 2026, the Association of Medicine and Psychiatry predicts a 22% rise in ECG monitoring for antipsychotic users. Telemedicine ECGs are making it easier for community patients to get checked without traveling to a cardiologist.
The message is clear: monitoring isn’t optional. It’s standard care.
What You Can Do
If you’re taking an antipsychotic:- Ask your doctor: “What’s my QTc? Has it been checked?”
- Know your meds. Bring a full list to every appointment.
- Don’t skip blood tests. Potassium and magnesium matter.
- If you feel dizzy, faint, or have palpitations-tell someone immediately.
If you’re a caregiver or family member:
- Help track medications and appointments.
- Watch for signs of irregular heartbeat or fainting.
- Don’t assume the doctor has checked everything. Ask.
The goal isn’t fear. It’s awareness. Antipsychotics save lives. But they need careful handling-like any powerful tool.
Can antipsychotics cause sudden cardiac death?
Yes, but it’s rare and usually happens when multiple risk factors are present-like high doses, other QT-prolonging drugs, low potassium, or existing heart disease. The absolute risk is low for most people, but it’s real enough that doctors now screen for it. Most cases are preventable with proper monitoring.
Which antipsychotic has the lowest risk of QT prolongation?
Lurasidone has the lowest risk, with studies showing near-background levels of QT prolongation. Aripiprazole, brexpiprazole, and paliperidone are also low-risk options. These are often preferred for patients with heart conditions or those taking other medications that affect the heart.
Do I need an ECG if I’m on a low-risk antipsychotic?
Even for low-risk drugs, a baseline ECG is recommended if you have other risk factors-like being over 65, female, having heart disease, or taking other medications that affect the QT interval. For healthy, young patients on a low-risk antipsychotic alone, annual checks may be enough. But don’t skip it entirely.
Can I take over-the-counter meds with antipsychotics?
Many OTC drugs can interfere. Antihistamines like diphenhydramine (Benadryl), certain cough syrups with dextromethorphan, and even some herbal supplements can prolong QT. Always check with your pharmacist or doctor before taking anything new-even if it’s sold without a prescription.
Is it safe to stop my antipsychotic if I’m worried about my heart?
No. Stopping abruptly can trigger psychosis, relapse, or even suicide. If you’re concerned about your heart, talk to your doctor. They can check your QTc, adjust your dose, or switch you to a safer medication. Never stop on your own.
How often should my QT interval be checked?
Baseline ECG before starting. Then within one week after reaching a stable dose if you’re on a moderate or high-risk drug. After that, annual checks are standard. If you have risk factors or change medications, more frequent monitoring may be needed.
Are there alternatives to antipsychotics for schizophrenia?
There are no equally effective alternatives for treating schizophrenia. Therapy and social support help, but they don’t replace medication for most people. The benefits of antipsychotics in reducing suicide and accidental death far outweigh the cardiac risks when used with proper monitoring.


10 Comments
Wow, this is one of the most comprehensive breakdowns of QT prolongation risks I’ve ever seen. 🙌 As someone who’s seen a close family member navigate antipsychotic treatment, I can’t stress enough how vital ECG monitoring is. The stats on potassium levels and polypharmacy? Chilling. But also empowering - knowledge is the best shield here. Keep sharing this kind of stuff. 💙
Let’s be honest - this is just another example of pharmaceutical companies pushing drugs with known cardiac risks because they’re profitable. The FDA’s TQT studies? A PR stunt. They don’t test long-term polypharmacy in real-world elderly populations. And yet, we’re told to trust the guidelines. Meanwhile, people are dying quietly in nursing homes while their charts say 'stable.' Don’t be fooled.
Look, I get the science. But let’s not pretend this isn’t just another way for the medical-industrial complex to keep people dependent. You wanna reduce cardiac risk? Stop giving people five meds at once. Stop letting psychiatrists prescribe without a cardiologist in the room. The real solution isn’t monitoring - it’s less polypharmacy. Period.
Just wanted to add - I’m a nurse in psych and we’ve started doing baseline ECGs for *everyone* on antipsychotics now, even low-risk ones if they’re over 50. The one time we didn’t, a patient had a near-code because their potassium was 3.1 and they were on quetiapine + citalopram. We caught it in time. But it was close. Always check electrolytes. Always.
Oh so now we’re supposed to believe that haloperidol is ‘moderate risk’ but diphenhydramine from Benadryl is the real villain? 😂 Tell me again why Big Pharma didn’t ban antihistamines from OTC shelves if they’re so dangerous? They’re making billions off both. This whole thing is a distraction so we don’t ask why we’re medicating people instead of housing them. And don’t even get me started on how often potassium gets ignored in hospitals. It’s not a medical issue - it’s a capitalism issue.
There is a profound tension here between the necessity of pharmacological intervention for severe mental illness and the ethical imperative to preserve physiological integrity. The data presented reveals not a failure of medicine, but a failure of systems - fragmented care, inadequate training, and the commodification of health outcomes. To reduce this to ‘risk vs benefit’ is to ignore the human context: a 72-year-old woman isn’t a statistical outlier - she is a mother, a veteran, a person who deserves coordinated, compassionate care. We must move beyond algorithmic prescribing toward integrative, patient-centered models that honor both mind and body as inseparable.
Thank you for writing this. Seriously. I’m a caregiver for my brother who’s on aripiprazole and I didn’t even know QT was a thing until last month. I asked his psychiatrist for his last ECG results and she looked at me like I’d asked for his DNA. We got it done at a free clinic. His QTc was 482. We switched meds. He’s doing better. If you’re reading this and you’re on any of these drugs - ask. Ask. Ask. It’s not being difficult. It’s being alive.
Baseline ECG required for all antipsychotics. No exceptions. Documentation mandatory. Failure to comply constitutes negligence.
While the article presents a commendable synthesis of current clinical guidelines, one cannot help but observe the troubling epistemological gap between evidence-based protocols and their implementation in under-resourced settings. The assertion that monitoring is 'standard care' presumes universal access to electrocardiographic technology, trained personnel, and longitudinal follow-up - conditions neither universally nor equitably realized. One must therefore interrogate the ideological underpinnings of such recommendations: are they truly clinical, or merely aspirational constructs of Western medical hegemony?
This isn’t just medicine - it’s a symphony of survival. Antipsychotics are the quiet heroes in the background, keeping minds from unraveling while the heart quietly sings its own dangerous tune. We don’t need to fear the drugs. We need to learn their rhythm. Check the ECG. Balance the salts. Talk to your pharmacist. Listen to your body. The goal isn’t to live without risk - it’s to live with awareness. And that, my friends, is the most radical act of self-care there is.