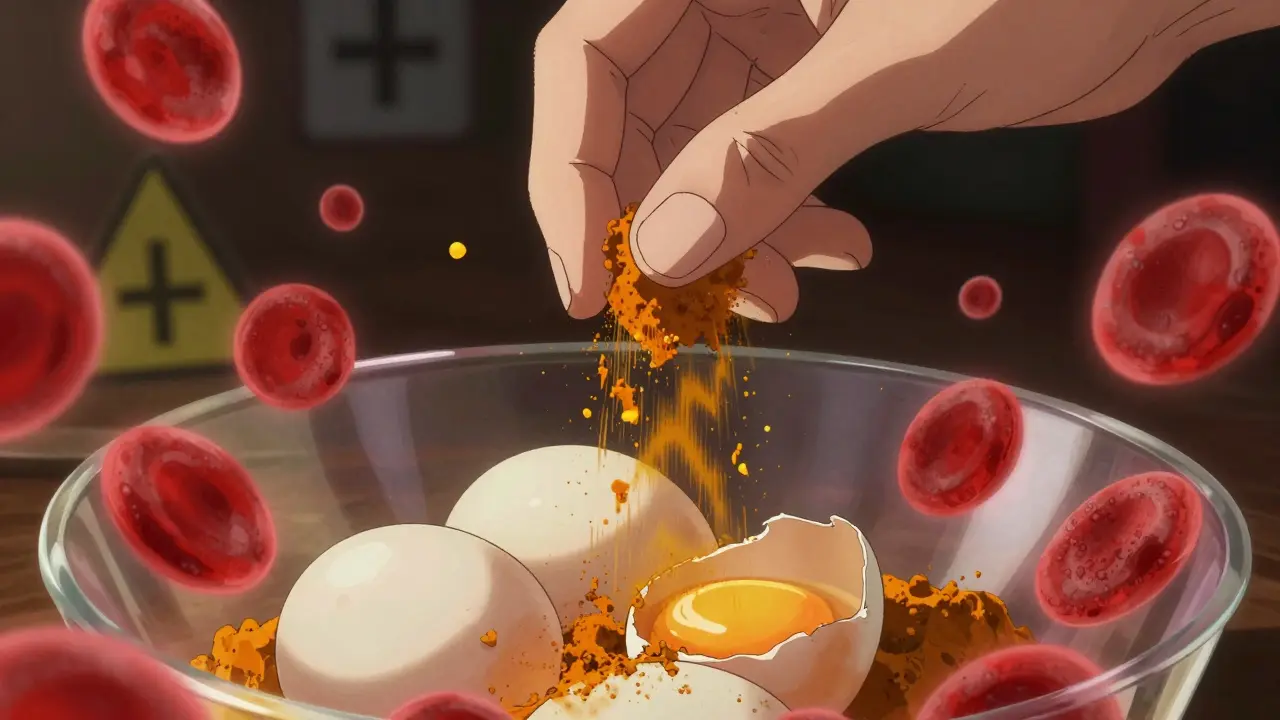
Many people take turmeric for its anti-inflammatory benefits, believing it’s just a harmless spice. But if you’re on a blood thinner like warfarin, aspirin, or rivaroxaban, that daily sprinkle on your eggs or turmeric capsule could be putting you at serious risk. The science is clear: turmeric and its active compound, curcumin, can dangerously amplify the effects of blood thinners - leading to uncontrolled bleeding, hospitalization, or even death.
How Turmeric Acts Like a Blood Thinner
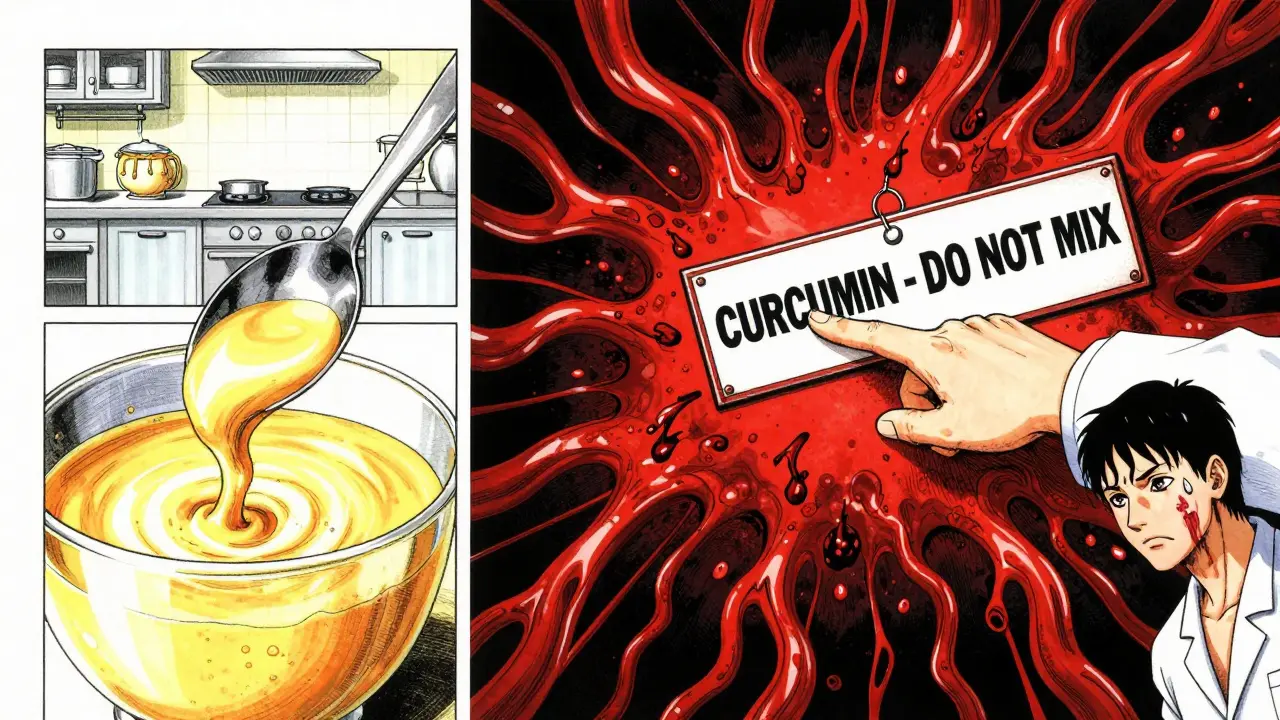
Turmeric isn’t just a spice. Its main active ingredient, curcumin, directly interferes with your body’s ability to form clots. Research shows curcumin inhibits two key clotting proteins: thrombin and factor Xa. These are the same targets of powerful prescription drugs like Xarelto and Eliquis. Unlike those medications, though, curcumin doesn’t come with a precise dose or monitoring system. A teaspoon of ground turmeric might contain 20-40 mg of curcumin. A supplement? That could be 500-1,500 mg - a 50x difference.Curcumin also reduces platelet aggregation, meaning your blood platelets - the sticky cells that form clots - become less likely to stick together. This is a double hit: it slows clotting through the coagulation cascade and weakens platelet function. The result? Longer bleeding times. A 2012 study published in PubMed found that both curcumin and its derivative BDMC significantly prolonged aPTT and PT - two standard lab tests used to measure blood clotting speed.
Real Cases of Dangerous Interactions
This isn’t theoretical. Real people have been hospitalized because of turmeric.In 2018, Medsafe in New Zealand reported a case where a patient on stable warfarin therapy had an INR (a blood test that measures clotting time) that suddenly jumped to over 10. The normal range for someone on warfarin is 2 to 3.5. An INR above 10 means the blood takes more than 10 times longer to clot than it should. This patient had started taking a turmeric supplement just weeks before. They were lucky - they didn’t bleed internally. But many aren’t.
Another case involved a kidney transplant patient who took 15 or more spoonfuls of turmeric powder daily for ten days. Their tacrolimus (a critical anti-rejection drug) levels spiked to 29 ng/mL - far above the safe range. Their kidneys were damaged. Why? Turmeric likely blocked the liver enzyme CYP3A4, which normally breaks down tacrolimus. This same enzyme is involved in metabolizing warfarin and other blood thinners. When turmeric slows its activity, drug levels build up - and so does the bleeding risk.
Which Blood Thinners Are Affected?
Turmeric doesn’t just interact with one type of blood thinner. It affects nearly all of them:- Warfarin (Coumadin): The most dangerous combo. Warfarin has a narrow therapeutic window - a tiny change in dose can cause bleeding or clotting. Turmeric pushes INR levels dangerously high.
- DOACs (rivaroxaban, apixaban, dabigatran, edoxaban): These newer drugs are often seen as safer, but turmeric still inhibits factor Xa - the same target. No one has proven it’s safe to mix them.
- Aspirin, clopidogrel (Plavix): These are antiplatelet drugs. Turmeric adds to their effect, increasing bruising and bleeding risk.
- Heparin, enoxaparin (Lovenox), dalteparin (Fragmin): Injectable anticoagulants. Turmeric can make their effects unpredictable and harder to control.
- NSAIDs like ibuprofen, naproxen, diclofenac: These already raise bleeding risk. Add turmeric, and you’re stacking the deck.
The British Heart Foundation and Mayo Clinic both warn that turmeric supplements can interfere with all these medications. Even if you’re not on warfarin, you’re not safe.

Why Supplements Are Riskier Than Spice
Eating turmeric in curry? Probably fine. The amount of curcumin in food is too low to cause major issues. But supplements? That’s a different story.Most turmeric powder contains only 2-8% curcumin. But concentrated supplements can be 95% curcumin. That’s like comparing a splash of vinegar to a bottle of pure acetic acid. One is a seasoning. The other is a chemical.
There’s no standardization. One brand’s 500 mg turmeric capsule might have 10 mg of curcumin. Another’s might have 475 mg. You can’t tell by looking. And no supplement is tested for interactions with blood thinners in large human trials. That’s why doctors say: avoid supplements entirely if you’re on anticoagulants.
What Doctors Say - And What You Should Do
The Welsh Medicines Information Centre updated their guidance in October 2024: curcumin may reduce how fast warfarin leaves your body, causing levels to rise. They stress: “Monitor closely if taken together.” But “monitor closely” is not enough. The Medsafe warning is clearer: “Concurrent use should be avoided.”Here’s what you need to do right now:
- If you’re on any blood thinner, stop taking turmeric supplements immediately.
- Don’t assume “natural” means safe. Turmeric is a potent bioactive compound - not a vitamin.
- Tell your doctor about every supplement you take, even if you think it’s harmless.
- If you’ve been taking turmeric and notice unusual bruising, nosebleeds, blood in urine or stool, or prolonged bleeding from cuts, get checked now.
- Stop turmeric supplements at least two weeks before any surgery - even a dental extraction.
The American Heart Association estimates 2-3% of adults in the U.S. and Europe take blood thinners. That’s millions of people. Many don’t realize turmeric is a risk. It’s not a myth. It’s not an old wives’ tale. It’s documented in medical journals, regulatory warnings, and real hospital cases.
What About Turmeric Tea or Cooking?
If you eat turmeric as a spice - a teaspoon in soup, curry, or golden milk - the curcumin dose is too low to cause harm in most people. The Welsh Medicines Information Centre notes that “it is unlikely that turmeric poses such risks when used in small quantities, as a spice.”But here’s the catch: if you’re on warfarin, even small amounts can matter. Your INR can be sensitive. If you’ve been eating turmeric regularly and your doctor suddenly changes your warfarin dose, they might not know why your numbers shifted. That’s why transparency matters. Tell your doctor if you use turmeric in food - especially if you’re having trouble keeping your INR stable.
Alternatives to Turmeric for Inflammation
If you’re taking turmeric for joint pain or inflammation, you need safer options. Here are evidence-backed alternatives that don’t interfere with blood thinners:- Omega-3 fatty acids (fish oil): Proven to reduce inflammation. Doses under 3 grams per day are generally safe with blood thinners - but check with your doctor first.
- Ginger: Has mild anti-inflammatory effects. Unlike turmeric, there’s little evidence it significantly affects clotting at culinary doses.
- Exercise and weight management: One of the most effective, drug-free ways to reduce chronic inflammation.
- Physical therapy or acupuncture: For joint pain, these have strong support in clinical guidelines.
None of these are perfect, but they’re far less risky than stacking turmeric on top of warfarin.
Final Word: Don’t Guess. Ask.
The biggest danger isn’t turmeric itself. It’s the assumption that because it’s natural, it’s safe to combine with medicine. It’s not. Blood thinners are some of the most dangerous drugs to mix with supplements. A single change in INR can mean the difference between life and death.If you’re on a blood thinner, don’t take turmeric supplements. Period. If you’re unsure, talk to your doctor or pharmacist - bring the bottle. Don’t rely on Google. Don’t rely on anecdotal advice. The evidence is clear, the cases are real, and the stakes are too high to risk it.


11 Comments
Wow. This is one of those posts that makes you stop scrolling and actually think. I’ve been taking turmeric capsules for my knees - thought it was just a ‘natural anti-inflammatory’ like they say on Instagram. Turns out I was playing Russian roulette with my blood. Thanks for the wake-up call. I’m dumping the supplements tomorrow. 🙏
I’m not even on blood thinners but I just threw out my entire turmeric stash. This isn’t just about meds - it’s about how we treat ‘natural’ like it’s harmless magic dust. It’s a drug. A potent one. And we treat it like a tea bag. That’s the real problem.
Brothers and sisters, I’m from Nigeria - we use turmeric in everything. Jollof rice, soups, even on our skin. But I’ve seen people collapse from bleeding after surgery because they kept taking their ‘healing powder’ without telling the doctor. This isn’t just Western medicine fear - it’s life. If you’re on any medicine that keeps you alive, don’t gamble with what you put in your body. Speak up. Tell your family. Tell your auntie who swears turmeric cures cancer. Love you all. Stay safe.
Excellent breakdown. The distinction between culinary use and pharmacological dosing is critical. Curcumin’s inhibition of CYP3A4 and factor Xa is well-documented in peer-reviewed pharmacokinetic studies. The lack of regulatory oversight in supplement manufacturing means dosage variability is not just possible - it’s guaranteed. This isn’t anecdotal; it’s biochemistry.
Let’s be real - the supplement industry thrives on ignorance. They slap ‘natural’ on a bottle and suddenly it’s immune to science. But turmeric isn’t a vitamin - it’s a bioactive compound with pharmacological effects. And people die because they think ‘it’s just a spice.’ The FDA doesn’t regulate supplements like drugs - that’s not a bug, it’s a feature of their business model. Don’t trust labels. Trust evidence.
As an American, I find it appalling that we allow such dangerous substances to be sold without warning labels. In Europe, this would be classified as a Class 2 drug interaction. Here? It’s just another $12 bottle on Amazon with 4.7 stars and 2,000 reviews from people who ‘feel more energized.’ This is negligence disguised as freedom. Someone needs to sue these companies.
Just wanted to add - if you’re on warfarin and you’ve been eating turmeric in food for years, don’t panic - but DO tell your doctor. INR can shift subtly, and your dose might need adjusting. I’m a pharmacist. I’ve seen this happen. A patient thought ‘a little curry’ was fine - but her INR went from 2.8 to 5.1 in two weeks. She had a nosebleed that wouldn’t stop. It’s not about fear. It’s about awareness. Always disclose everything - even the ‘harmless’ stuff.
OH MY GOD. I’ve been giving my mom turmeric capsules for her arthritis - she’s on Eliquis. I just threw them out. I feel like such an idiot. I thought she was being ‘healthy.’ I didn’t know. I’m so sorry, Mom. I’m crying right now. This could’ve killed her. Thank you for posting this. I’m sharing this with everyone I know.
Been on Xarelto for 3 years. Took turmeric for a month last year because of back pain. Didn’t feel anything - no bruising, no bleeding. But after reading this, I’m done. Better safe than sorry. Also, ginger tea is now my new best friend. 🍵✌️
My grandma used to put turmeric in everything - she’s 89 and still walks two miles a day. She never took supplements. Maybe the real lesson here is: eat it in food, not in pills. And listen to your body - if something feels off, check with your doctor. Simple.
So if I eat curry, I’m fine? But if I take a pill, I’m a dumbass? That’s messed up. Who decided that? Why can’t I just take a pill like normal people? This is why I hate American doctors. Always making things complicated.