For people with kidney disease, what seems like a simple fix for heartburn can turn into a medical emergency. Over-the-counter antacids like Tums or Milk of Magnesia are everywhere - easy to grab, cheap, and fast-acting. But if your kidneys aren’t working right, these common meds can cause serious harm. The problem isn’t just acid reflux. It’s phosphate. And the wrong antacid can push your blood chemistry into dangerous territory - leading to heart problems, bone damage, or even death.
How Antacids Work in Kidney Disease
Antacids were never meant to be kidney medicines. They were designed to neutralize stomach acid. But in the 1980s, doctors noticed something unexpected: calcium and aluminum in antacids stuck to phosphate in the gut, stopping it from entering the bloodstream. That’s when they started using them as phosphate binders for people with chronic kidney disease (CKD). When kidneys fail, they can’t flush out phosphate. Levels rise. High phosphate doesn’t just cause itching - it pulls calcium out of your bones, hardens your arteries, and increases your risk of heart attack. That’s why phosphate control is critical. For people with CKD stage 3 or higher, keeping serum phosphate between 2.7 and 4.6 mg/dL is the goal, according to KDIGO guidelines. Calcium carbonate (Tums) and aluminum hydroxide (Alu-Cap) became go-to options because they bind phosphate well. But here’s the catch: they’re not safe for everyone. And they’re not interchangeable with prescription binders like sevelamer or lanthanum carbonate.The Three Big Risks: Calcium, Aluminum, Magnesium
Not all antacids are created equal. Each type carries different dangers for people with kidney disease. Calcium-based antacids (like Tums or calcium citrate) are cheap and widely used. But they add extra calcium to your body. Your kidneys normally regulate calcium, but when they’re damaged, calcium builds up. Levels above 10.2 mg/dL raise your risk of vascular calcification - calcium deposits in your heart and blood vessels. A 2019 study in the Journal of the American Society of Nephrology found that CKD patients with calcium levels over 10.2 mg/dL had a 30-50% higher chance of heart-related events. That’s why many nephrologists stop calcium antacids once GFR drops below 30 mL/min. Aluminum-based antacids (like Maalox or Amphojel) are even more dangerous. Aluminum doesn’t leave the body easily when kidneys are weak. It builds up in bones, causing pain and fractures. It crosses into the brain, leading to dementia-like symptoms called dialysis encephalopathy. The FDA banned long-term aluminum use in 1990. Today, it’s only allowed for short-term rescue therapy - never as a daily binder. Serum aluminum above 60 mcg/L is toxic. Above 40 mcg/L, it starts damaging bones. Magnesium-based antacids (like Milk of Magnesia) are often used for constipation. But magnesium is cleared by the kidneys. When kidney function falls below 10 mL/min, magnesium builds up. Levels above 4 mg/dL cause muscle weakness. Above 10 mg/dL, it can paralyze your breathing or stop your heart. Emergency rooms see this often - patients on dialysis who took milk of magnesia for constipation and ended up in ICU.Prescription Binders vs. Over-the-Counter Antacids
Prescription phosphate binders like sevelamer (Renagel), lanthanum carbonate (Fosrenol), and sucroferric oxyhydroxide (Velphoro) were developed to solve the problems of antacids. Sevelamer doesn’t contain calcium or aluminum. It binds phosphate without raising blood levels. It’s more expensive - about $2,000 a month - but safer. Studies show it reduces hypercalcemia risk by 40% compared to calcium carbonate in stage 4 CKD patients. Lanthanum carbonate works similarly, but costs even more - up to $3,500 monthly. Velphoro has fewer pills to take (1-2 per meal vs. 4-6 for calcium carbonate), but costs around $4,000 a month. Antacids win on price. Calcium carbonate costs about $10 a month. That’s why many low-income patients rely on it. But cost savings can turn into hospital bills. A 2022 study found that 57% of antacid-related ER visits in CKD patients involved aluminum or magnesium products used without medical guidance.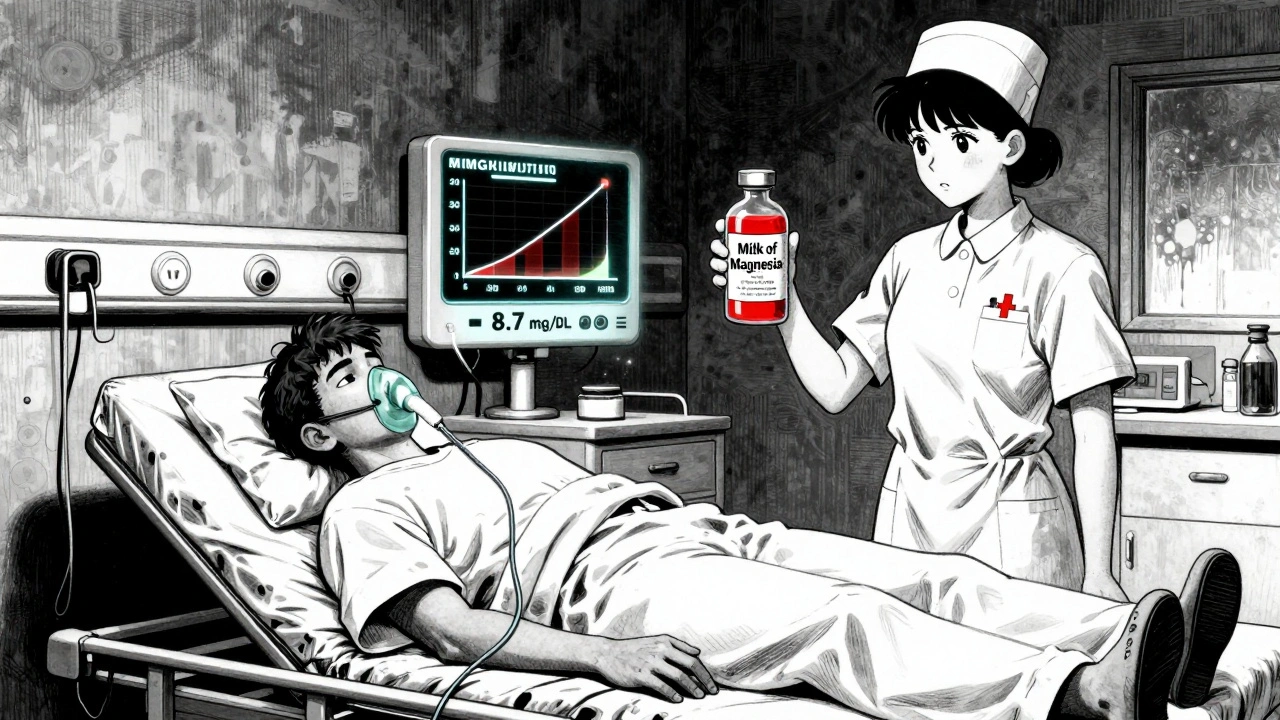
Who Should Use Antacids - And Who Should Avoid Them
There’s no one-size-fits-all answer. It depends on your kidney function.- CKD Stage 3 (GFR 30-59): Calcium carbonate may be used under supervision. Dose: 600-1200 mg elemental calcium per meal. Monitor calcium monthly. Avoid aluminum and magnesium completely.
- CKD Stage 4-5 (GFR <30): Avoid all antacids as phosphate binders. Use only prescription binders. If you need heartburn relief, calcium carbonate is the only option - and only if taken at least 2 hours before or after your phosphate binder. Never take magnesium or aluminum.
- Dialysis patients: Do not use magnesium or aluminum antacids. Even small doses can be fatal. Calcium carbonate should be used sparingly and only with doctor approval.
Drug Interactions You Can’t Ignore
Antacids don’t just affect phosphate. They mess with other meds. They can reduce absorption of antibiotics like ciprofloxacin, thyroid meds like levothyroxine, and seizure drugs like phenytoin. One study showed phenytoin levels dropped by 40% when taken with antacids. That means seizures could return. The Cleveland Clinic recommends taking other medications either one hour before or four hours after an antacid. If you’re on multiple pills, write down your schedule. Ask your pharmacist to review it.Real Stories: What Happens When People Don’t Know the Risks
A 62-year-old woman in Ohio took Tums daily for heartburn for six months. She had CKD stage 4. Her calcium level hit 11.2 mg/dL. A CT scan showed calcium deposits in her coronary arteries. She needed stents. A man in Florida used Milk of Magnesia for constipation. His magnesium level rose to 8.7 mg/dL. He lost movement in his legs and was rushed to the ER. He spent three days on a ventilator. These aren’t rare. The American Association of Kidney Patients surveyed 1,200 CKD patients in 2022. 68% couldn’t tell the difference between a prescription phosphate binder and an over-the-counter antacid. 42% had used antacids without telling their nephrologist.
What You Should Do
If you have kidney disease:- Never take an antacid without asking your nephrologist.
- Know what’s in your antacid. Check the label for calcium carbonate, aluminum hydroxide, or magnesium hydroxide.
- Don’t use antacids as your main phosphate binder unless your doctor says so.
- Get monthly blood tests: calcium, phosphate, magnesium, and aluminum (if you’ve used aluminum products).
- Know the warning signs: nausea, confusion, muscle weakness, trouble breathing, bone pain, or seizures.
- If you’re on dialysis, avoid magnesium and aluminum entirely.
What’s Changing Now
New drugs are coming. Tenapanor (Xphozah), approved in 2023, doesn’t bind phosphate - it blocks its absorption in the gut. It’s a pill, not a powder. Fewer doses. Less risk of overdose. The NIH is running a five-year study called ASK-D, tracking 5,000 CKD patients to build better guidelines. The FDA is pushing for clearer labels on antacids - possibly separating "heartburn relief" from "phosphate binder" versions by 2025. Clinics are launching education programs. The American Nephrology Nurses Association’s "Know Your Binders" campaign has already cut inappropriate antacid use by 28% in pilot clinics.The Bottom Line
Antacids aren’t harmless. For people with kidney disease, they’re a ticking time bomb if used wrong. Calcium carbonate can be a tool - but only under strict supervision. Aluminum and magnesium? Avoid them. Always. Prescription binders are safer, even if they cost more. Your kidneys can’t handle the extras. And neither can your heart, bones, or brain. If you’re unsure what you’re taking - or why - ask your nephrologist. Bring your medicine cabinet. Show them every bottle. Don’t assume "over-the-counter" means "safe."Can I take Tums if I have kidney disease?
You may take calcium carbonate (Tums) only if your nephrologist approves it. It’s sometimes used as a phosphate binder in early-stage kidney disease (CKD stage 3), but only at specific doses and with monthly blood tests. Avoid it entirely if your GFR is below 30 mL/min or if you’re on dialysis, unless specifically directed. Never use it as a long-term solution without supervision.
Is Milk of Magnesia safe for kidney patients?
No. Milk of Magnesia contains magnesium hydroxide, which can cause life-threatening hypermagnesemia in people with kidney disease. Even small doses can lead to muscle weakness, low blood pressure, breathing problems, or cardiac arrest. It should be avoided completely in CKD stages 4 and 5, and used with extreme caution - if at all - in stage 3. Always consult your nephrologist before using it.
Why are aluminum antacids dangerous for kidney disease?
Aluminum builds up in the body when kidneys can’t remove it. This leads to aluminum toxicity, which causes bone pain, fractures, brain damage (dialysis dementia), and microcytic anemia. The FDA restricts aluminum antacids to a maximum of two weeks of use in people with normal kidneys. For those with CKD, they’re considered unsafe and are only used in rare, emergency situations under strict monitoring.
What are the signs of high calcium from antacids?
Symptoms include nausea, vomiting, constipation, excessive thirst, frequent urination, confusion, fatigue, and bone pain. High calcium can also lead to kidney stones and calcification in your heart and blood vessels. If you have kidney disease and experience these symptoms after taking antacids, get your calcium level checked immediately.
Can antacids interfere with my other medications?
Yes. Antacids can reduce how well your body absorbs antibiotics, thyroid medication, seizure drugs like phenytoin, and iron supplements. To avoid this, take other medications at least one hour before or four hours after an antacid. Always tell your pharmacist and doctor what antacids you’re using.
Are there safer alternatives to antacids for heartburn with kidney disease?
Yes. H2 blockers like famotidine (Pepcid) or proton pump inhibitors like omeprazole (Prilosec) are safer for heartburn in kidney disease patients because they don’t affect phosphate or electrolytes. However, even these should be used under medical supervision, especially in advanced CKD. Always ask your doctor before starting any new medication for heartburn.







8 Comments
Just took a look at my Tums bottle and realized I’ve been using it for heartburn for years… and I have stage 3 CKD. 😳 I’m calling my nephrologist tomorrow. Thanks for the wake-up call - this could’ve been deadly.
Let’s be real - if you’re taking OTC antacids without knowing the phosphate content, you’re not managing your CKD, you’re playing Russian roulette with your vasculature. The fact that people still think ‘over-the-counter’ = ‘safe’ is why healthcare costs are exploding. I’ve seen three patients in the last year with aluminum toxicity because they ‘just needed something for acid.’ No. Just no.
wait… so you’re telling me the government lets them sell poison in the same aisle as gum and candy? 🤔 maybe the pharma companies are hiding the truth… or maybe the FDA is in on it? i read somewhere that calcium is actually good for you and this whole thing is a scam to sell expensive binders. 🤷♂️
Hey everyone - I’m a dialysis nurse and I see this every single week. Someone comes in with magnesium toxicity because they took Milk of Magnesia for constipation. 💔 It’s heartbreaking. Please, if you have kidney disease, keep a list of meds in your wallet. Show it to every provider. You’re not being annoying - you’re saving your life. 💙🩺
Anyone who thinks sevelamer is worth $2,000 a month hasn’t done the math on ICU bills. The real issue isn’t the cost of binders - it’s the lack of basic medical literacy. If you can’t read a drug label, maybe you shouldn’t be self-medicating. This isn’t a conspiracy. It’s biology. And biology doesn’t care how much you ‘believe’ in natural remedies.
I had no idea aluminum could wreck your brain. My grandma took Maalox for 15 years. She started forgetting names, then her hands shook… we thought it was just aging. Now I think it was aluminum dementia. I’m going through her medicine cabinet tonight. This post changed everything.
Just wanted to say thank you for writing this. My mom’s on dialysis and I’ve been terrified to ask her about her antacids - didn’t want to sound like I was accusing her. But now I know what to look for. I’m printing this out and we’re going to the pharmacy together this weekend. You made me feel less alone in this.
The tragedy isn’t just the medical risk - it’s the systemic failure. We allow dangerous OTC drugs to be marketed as ‘safe’ for chronic conditions while denying affordable prescription alternatives to low-income patients. This isn’t about individual negligence. It’s about a healthcare system that treats convenience as a substitute for care. Until we fix that, people will keep dying because they chose the $10 option over the $4,000 one - and nobody held the system accountable.