Every year, millions of older adults are prescribed benzodiazepines for anxiety or insomnia. Drugs like Xanax, Valium, and Ativan seem like a quick fix-until they aren’t. For seniors, these medications don’t just help. They harm. And the risks aren’t just possible-they’re well-documented, preventable, and often ignored.
Why Benzodiazepines Are Dangerous for Older Adults
Benzodiazepines work by boosting GABA, a calming neurotransmitter in the brain. That sounds good-until you’re 75. As people age, their bodies process drugs differently. The liver slows down. The brain becomes more sensitive. Even small doses can cause big problems.Seniors on benzodiazepines are 50% more likely to suffer a hip fracture. Why? The drugs cause dizziness, slow reaction times, and poor balance. One study found that the risk of a car crash while on these meds is the same as driving with a blood alcohol level of 0.05%-legally drunk in most states.
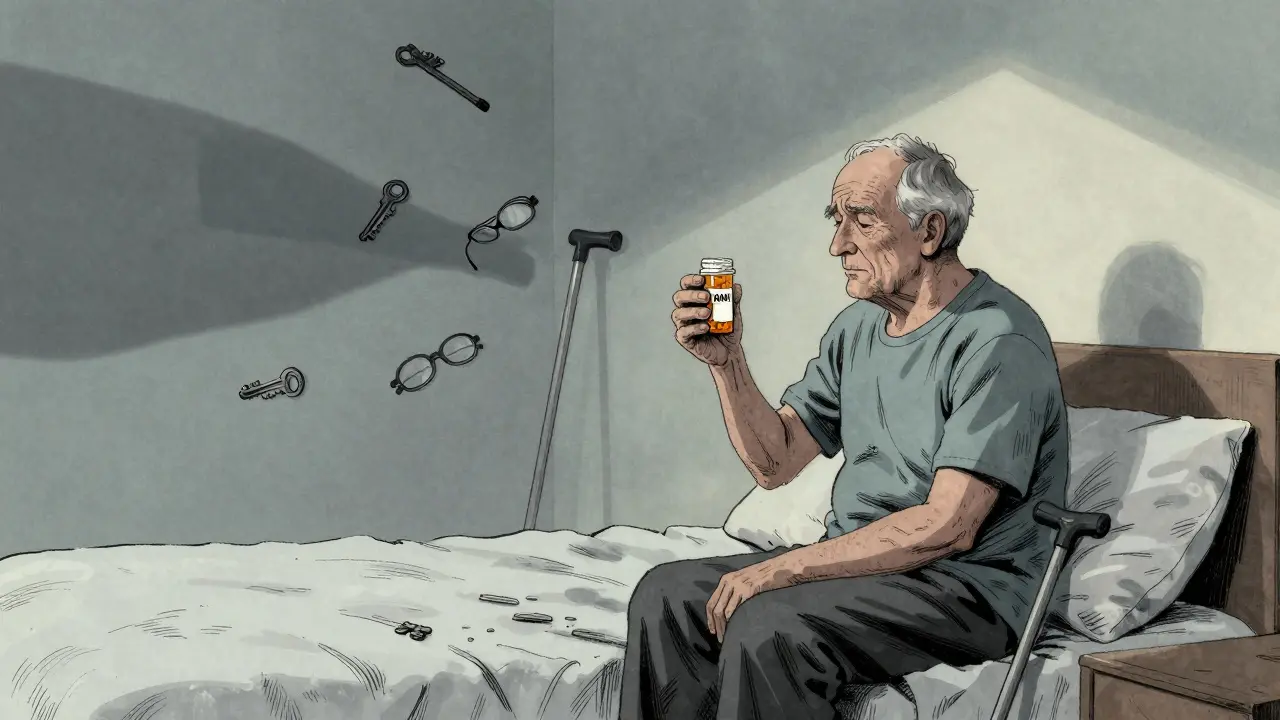
Memory loss is another major concern. Benzodiazepines block the brain’s ability to form new memories. This isn’t just forgetting where you put your keys. It’s forgetting names, appointments, even recent conversations. And it doesn’t go away when you stop taking the drug. Research shows cognitive decline can last for months after discontinuation.
But the scariest risk? Dementia. A 2023 study found that seniors who took benzodiazepines for 3 to 6 months had a 32% higher chance of developing Alzheimer’s. If they took them for more than six months? The risk jumped to 84%. Long-acting drugs like Valium and Librium are especially dangerous because they build up in the body over time. Even short-term use increases the risk.
The Myth of "Just a Little Help"
Many seniors believe their doctor prescribed benzodiazepines because they’re safe. That’s a dangerous assumption. The American Geriatrics Society’s Beers Criteria-used by doctors nationwide-has listed benzodiazepines as potentially inappropriate for older adults since 2012. The 2019 update made it even clearer: avoid them entirely, unless there’s no other option.Doctors aren’t always aware of the guidelines. Patients aren’t told the full story. A 2015 study found that only 32% of seniors knew benzodiazepines could impair their thinking. Just 41% knew they increased fall risk. Most thought the only danger was addiction-which is true, but only part of the picture.
On Reddit, a nurse shared that 9 out of 10 elderly patients she sees think their Xanax is harmless because it’s "prescribed." That’s not confidence-it’s misinformation. And it’s costing lives.
What Happens When You Stop?
Stopping benzodiazepines isn’t simple. The body gets used to them. Suddenly cutting off the drug can trigger withdrawal: anxiety spikes, insomnia returns worse than before, tremors, even seizures. That’s why quitting cold turkey is dangerous.But here’s the good news: you can stop safely-with the right plan. The American Society of Addiction Medicine recommends tapering slowly: reduce the dose by 5-10% every 1 to 2 weeks. For some, that takes 8 weeks. For others, it takes a year. The key is patience and support.
Studies show that combining tapering with cognitive behavioral therapy (CBT) doubles your chances of success. People who use CBT to manage anxiety or sleep issues while tapering are 65% more likely to quit successfully than those who just reduce the dose.
And yes, withdrawal symptoms are real. About 60-80% of seniors experience them. But they’re temporary. The fog lifts. Balance returns. Memory improves. The alternative-staying on the drug-is far worse.

Safer Alternatives for Anxiety and Insomnia
There are better ways to manage anxiety and sleep problems in older adults. None of them come with the same risks.Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It doesn’t involve pills. It teaches you how to reset your sleep habits-what to avoid before bed, how to handle racing thoughts, how to create a calm routine. Studies show 70-80% of seniors improve significantly. And the benefits last for years, not weeks.
Medicare started covering CBT-I in 2022. Yet only 12% of eligible seniors use it. Why? Lack of awareness. Limited providers. But it’s available. And it works.
SSRIs and SNRIs like sertraline or venlafaxine are first-line treatments for anxiety in seniors. They take 4 to 6 weeks to work, but they don’t cause drowsiness, falls, or memory loss. They’re not addictive. And they’ve been used safely in older adults for decades.
Ramelteon is a melatonin receptor agonist approved for sleep onset. It doesn’t cause dependence or cognitive side effects. It’s not a miracle cure for staying asleep, but it’s far safer than anything in the benzodiazepine family.
Avoid antihistamines like diphenhydramine (Benadryl). They’re often sold as "sleep aids," but they block acetylcholine-a brain chemical critical for memory. Long-term use increases dementia risk by up to 50%. That’s not a sleep aid. It’s a brain risk.
What You Can Do Right Now
If you or a loved one is on a benzodiazepine, don’t panic. But don’t wait either.- Ask your doctor: "Is this still necessary?"
- Request a review of all medications-especially if they’ve been on it for more than 3 months.
- Ask about CBT-I or a referral to a geriatric psychiatrist.
- Don’t stop suddenly. Work with your provider on a taper plan.
- Use tools like the Beers Criteria checklist to track which drugs are risky.
Some families worry about "making things worse" by stopping the med. But the truth is: the med is already making things worse. The fog, the falls, the memory lapses-they’re not aging. They’re the drug.
What’s Changing in 2025 and Beyond
The tide is turning. In January 2025, Medicare launched the Beers Criteria Action Plan. Its goal? Cut inappropriate benzodiazepine prescribing by 50% by 2027. Pharmacies now flag risky prescriptions. Doctors get alerts when they write them.The FDA updated benzodiazepine labels in April 2024 to include clear warnings about dementia risk. That’s huge. For the first time, the warning is on every bottle.
Researchers are testing new ways to help seniors quit. The NIH-funded BRIGHT trial, launched in late 2024, uses telehealth coaching to guide deprescribing. Results won’t be ready until 2029-but early feedback shows promise.
The American Geriatrics Society now lists benzodiazepine deprescribing as one of its top five priorities for 2025-2027. That means more training, more resources, more support.
Final Thought: It’s Not About Willpower
This isn’t about being strong enough to quit. It’s about being smart enough to choose safer options. Benzodiazepines were never meant for long-term use in older adults. They were designed for short-term crises: a panic attack before surgery, acute trauma, or end-of-life distress.Using them for months or years? That’s not treatment. That’s a gamble with your brain, your balance, your independence.
The alternatives exist. The evidence is clear. The guidelines are updated. The risks are real. And the clock is ticking.
Are benzodiazepines ever safe for seniors?
Benzodiazepines may be used briefly-days to a few weeks-in rare cases like severe panic attacks, acute alcohol withdrawal, or end-of-life care. But they are not safe for ongoing anxiety or insomnia in older adults. The American Geriatrics Society and FDA both warn against long-term use due to high risks of falls, cognitive decline, and dementia.
How long does it take to taper off benzodiazepines safely?
Most seniors need 8 to 16 weeks to taper safely, reducing by 5-10% every 1-2 weeks. For those on high doses or long-term use, tapering over 6 to 12 months may be necessary. Going too fast can cause dangerous withdrawal symptoms. Always work with a doctor who understands geriatric deprescribing.
Can CBT-I really replace sleeping pills for seniors?
Yes. CBT-I is the most effective long-term treatment for insomnia in older adults. Studies show 70-80% of seniors improve significantly, with benefits lasting years. Unlike pills, CBT-I doesn’t cause drowsiness, memory loss, or falls. Medicare now covers it, but access is still limited due to provider shortages.
Why are antihistamines like Benadryl dangerous for seniors?
Antihistamines like diphenhydramine block acetylcholine, a brain chemical vital for memory and thinking. Long-term use increases dementia risk by up to 50%. They also cause dry mouth, constipation, confusion, and urinary retention. They’re not safe sleep aids-they’re brain risks disguised as over-the-counter remedies.
What should I do if my doctor won’t help me stop benzodiazepines?
Ask for a referral to a geriatrician or a pharmacist specializing in medication reviews. Many hospitals and clinics now have deprescribing programs. You can also contact the Benzodiazepine Information Coalition for free resources and peer support. Your health matters more than a doctor’s habit.







13 Comments
I saw my dad on Xanax for 18 months after Mom passed. He was falling constantly, forgetting birthdays, barely eating. We didn’t know it was the drug until his geriatrician pulled it up on the Beers Criteria list. Took him 9 months to taper. He’s sleeping better now, walking without a cane, remembers my kid’s name. This isn’t hype-it’s survival.
Oh wow so now we’re blaming the drugs and not the fact that old people just get dumb? Maybe they shouldn’t be driving or living alone if their brains are fried from age and bad choices. At least the pills made them chill.
CBT-I works. I helped my mom through it last year. No pills. Just sleep restriction, stimulus control, and learning to stop fighting the wakefulness. She was skeptical. Now she says she feels more in control than she has in years. Medicare covers it but you gotta push. Call your local Area Agency on Aging-they’ll hook you up with a provider. It’s not magic. It’s science.
Oh sweet Jesus. Another one of these ‘benzos are evil’ sermons. Let me guess-you’re the type who thinks grandma should meditate through her panic attacks while balancing on one foot? Wake up. Sometimes the only thing keeping someone from screaming into a pillow is a tiny white pill. And if that pill lets them sleep, eat, and not cry all day? That’s not a crime. That’s mercy.
Also, CBT-I? Try finding a therapist who takes Medicare and doesn’t charge $300/hour. Good luck, Karen.
I’m a nurse in a senior center. I’ve seen the fall after the fall after the fall. I’ve held hands while people sobbed because they forgot their own wedding day. I’ve watched families cry when they realize the ‘calm’ their loved one had was just chemical fog. This isn’t about being anti-pill. It’s about being pro-living. The alternatives aren’t perfect, but they’re alive. And so are they.
you know what the real problem is? people think they can fix aging with therapy. like its some kind of glitch. but death is the only real cure. and even then, its just a pause. benzos? they just make the silence softer. why fight the inevitable? we all end up lost in our own heads anyway.
I’m from the Philippines and we don’t have access to CBT-I or geriatric psychiatrists. My aunt took valium for 12 years because it was the only thing available. We didn’t know it was dangerous. Now she’s 80 and her balance is shot. But we didn’t have a choice. This post feels like it’s written for people with good healthcare. What about the rest of us?
So the FDA finally added a warning? Took them 50 years. Meanwhile, Big Pharma made billions off seniors’ fear. And now you want us to believe they’re suddenly on our side? Please. The system doesn’t care about you. It cares about profit. CBT-I? Sure. If you’re rich. Otherwise? Keep taking the pills. At least they don’t judge you for being old.
My grandma quit benzos last year. We did it slow-like, 5% every three weeks. She cried a lot. She had nightmares. But now? She’s baking pies again. She remembers my birthday. She dances in the kitchen to old Motown. That’s not a miracle. That’s her brain coming back to life. And yeah, it was hell. But the alternative? Watching her fade slowly into a fog? No thanks.
benzos are fine if you dont have alzheimers in your family
my uncle was on ativan for 7 years. doctor said it was fine. he died after a fall. we never knew it was the med. i just wish someone had told us sooner.
Oh wow, a 2023 study? How quaint. I’m sure the peer-reviewed literature from 1998 didn’t already prove this. I mean, why bother with actual clinical experience when you’ve got a shiny new journal article? Also, CBT-I? Cute. Try telling that to someone who can’t get out of bed because their anxiety is a live wire.
My mom’s on lorazepam. She says it’s the only thing that lets her sleep. She’s 82. I don’t want to take it away. But I also don’t want her to break her hip. What do I do? I’m so torn.