Every year, the U.S. Food and Drug Administration (FDA) issues dozens of safety notices about medications already on the market. These aren’t recalls or panic alerts-they’re detailed updates that can change how your doctor prescribes your drug, what side effects you should watch for, or even whether you should keep taking it. If you’re on a medication that’s been around for a while, you’re likely affected by one of these. But reading them? Most people skip them. That’s a mistake.
What Are FDA Safety Communications?
FDA Drug Safety Communications are official updates issued when new risks are discovered after a drug has been approved. They’re not warnings about manufacturing defects or counterfeit pills. These are about real, science-backed changes in how a medication works in the body-risks that only show up after thousands or millions of people have used it.
Since 2007, the FDA has had stronger legal power to track these risks through programs like the Sentinel Initiative, which analyzes health data from over 200 million patients. Between 2020 and 2023, they issued an average of 60 major safety communications per year. That’s one every six days. Some affect just one drug. Others change guidelines for entire classes-like all opioids or all blood thinners.
Where to Find Them
You won’t see these in your pharmacy’s waiting room. They’re published online at fda.gov/drugs/drug-safety-and-availability. But you don’t have to hunt for them.
The FDA offers free email alerts. You can sign up to get notifications only for the drugs you take-whether it’s your blood pressure pill, diabetes medication, or antidepressant. Just go to the website, scroll to the bottom, and choose your categories. No login. No subscription fee. No spam.
Pharmacists and doctors often get these alerts too, but they’re busy. If you’re the one taking the pill, you’re the one who should know the latest safety info.
How to Read One (Step by Step)
Let’s say you open a communication titled: "Updated Labeling for Opioid Medications: Risk of Withdrawal and Dependence". Here’s what to look for, in order.
- What Safety Concern Is FDA Announcing? This is the headline. It tells you the problem in plain language. In this case: "Do not suddenly stop taking opioids if you’ve been using them for a while. You could have dangerous withdrawal symptoms."
- For Health Care Professionals This section has technical details: which prescribing sections were changed (e.g., "2.x, 5.x"), what wording was added or removed (shown with bold and strikethrough), and whether it applies to all opioids or just one brand. It also references clinical studies that led to the change.
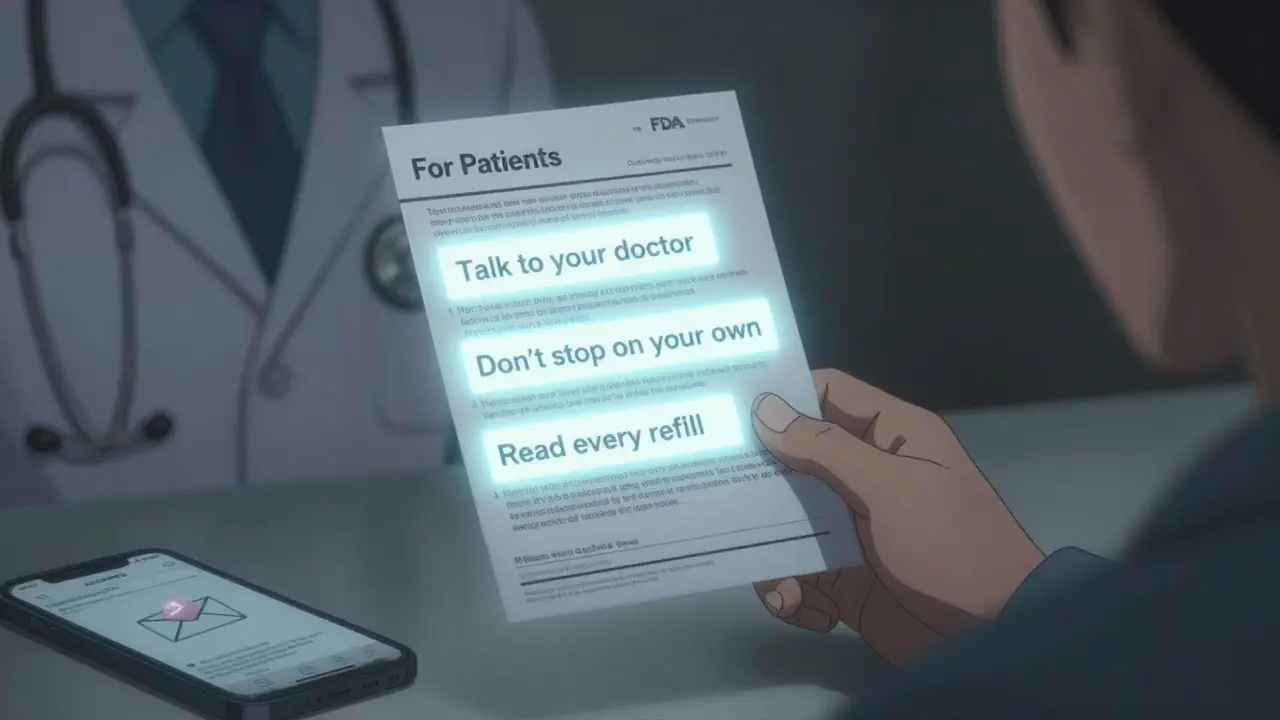
- For Patients This is your section. It says what you need to do: "Talk to your doctor before changing your dose," "Don’t stop on your own," "Read your Medication Guide every time you refill." It’s written in simple language, often at an 8th-grade reading level.
- Highlights of Prescribing Information This is a quick summary of major changes. Look for "Boxed Warning" updates-that’s the FDA’s strongest safety flag. If it’s there, the risk is serious enough to be printed in bold at the top of the drug’s official prescribing guide.
- What Changed in the Label? The FDA shows you exactly what old text was replaced with new text. If your pill’s label says "Use with caution in elderly patients," and now it says "Avoid use in patients over 75," that’s a big deal. You need to know.
Don’t skip the "For Patients" section. It’s the only part written for you.
What to Do When You See a Communication
Not every update means you need to stop your medication. But you should act.
- If the communication says "STOP using this medication immediately," call your doctor or pharmacist right away. Don’t wait.
- If it says "Consider this information when prescribing," or "Updated labeling," then schedule a check-in. Ask: "Does this change affect me? Should we adjust my dose or switch drugs?"
- If it mentions a "Medication Guide," find it. Every FDA-approved drug comes with one. It explains side effects, storage, and what to do if you miss a dose. If you haven’t read yours in over a year, read it now.
Some changes are subtle. For example, a 2022 update to the drug Copiktra (duvelisib) didn’t say "don’t take it." It said: "Patients may have a higher risk of serious infections. Talk to your doctor about whether you need additional vaccines." That’s not an emergency-but it’s something you need to discuss.
Common Confusions
There are different types of FDA notices. Don’t mix them up.
- Drug Safety Communication - Full update with detailed changes. This is the one you should read.
- Drug Alert - Short notice about an urgent issue. Often about a single batch or rare side effect. Still important, but less detailed.
- Drug Recall - The product is pulled from shelves. This is rare. If you hear about a recall, check the FDA site for the exact lot number.
- Labeling Change - The drug’s official instructions were updated. This usually follows a safety communication.
Many patients confuse alerts with recalls. An alert doesn’t mean your pills are unsafe. It means the FDA has new data-and you need to know what it means for you.

Why This Matters
Medications are safer than ever, but they’re not risk-free. The FDA doesn’t approve drugs because they’re perfect. They approve them because the benefits outweigh the risks. But those risks can change over time.
A 2021 study found that 63% of patients didn’t know the difference between a safety communication and a recall. Another study showed that only 37% of primary care doctors read full communications-mostly because they’re long and hard to digest.
That’s why the FDA is changing how they’re written. Since 2023, they’ve started testing plain-language summaries for high-risk drugs. These are short, visual, and available in Spanish too. You can find them on the same page as the full communication.
And here’s the truth: your doctor doesn’t always know about every update. A 2023 survey found that only 32% of electronic health record systems automatically include FDA alerts. So if you don’t check, no one else will.
What You Can Do Today
You don’t need to be a scientist to understand these. Here’s your action plan:
- Find out what drugs you’re taking. Write them down.
- Go to fda.gov/drugs/drug-safety-and-availability.
- Click "Subscribe to Email Alerts." Choose your drug classes (e.g., "Opioids," "Antidepressants").
- When you get an alert, open the "For Patients" section. Read it. Then call your doctor with one question: "Does this affect me?"
- Keep your Medication Guides. Don’t throw them away. Re-read them every time you refill.
It takes five minutes. But it could save you from serious side effects-or even a hospital visit.
What’s Coming Next
The FDA plans to start sending personalized safety alerts directly through patient portals by 2025. Imagine getting a message in your MyChart app: "Your blood thinner, Xarelto, now has a new warning about bleeding risk in patients over 70. Read more."
But until then, you’re your own best advocate. Don’t wait for your doctor to tell you. Don’t assume your pill is safe because it’s been on the market for years. Drugs change. So should your knowledge.
Are FDA Safety Communications the same as drug recalls?
No. A drug recall means the product is pulled from shelves due to contamination, mislabeling, or manufacturing defects. FDA Safety Communications are about new safety information discovered after a drug has been used for years-like unexpected side effects or changes in how it should be dosed. You don’t need to stop taking the drug unless the communication specifically says to.
How often does the FDA issue these communications?
The FDA issues 50 to 70 major Drug Safety Communications each year. That’s about one every six days. Some are about single drugs, others affect entire classes like opioids, blood thinners, or diabetes medications. The number has increased since 2007, when the FDA gained stronger legal authority to monitor drug safety after approval.
What should I do if I see a "Boxed Warning" in a safety communication?
A Boxed Warning is the FDA’s strongest safety alert. It means the drug carries a serious, potentially life-threatening risk-like liver damage, heart failure, or suicidal thoughts. Don’t panic. Don’t stop the drug on your own. Call your doctor immediately. Ask: "Is this risk relevant to me? Should we adjust my dose or switch medications?"
Do I need to read the full FDA communication?
Not unless you’re a doctor or pharmacist. For patients, the "For Patients" section is all you need. It’s written in plain language, summarizes the key changes, and tells you exactly what to do. The rest of the document is for healthcare providers. If you’re unsure, share the "For Patients" part with your doctor and ask for clarification.
Can I trust the information in FDA communications?
Yes. The FDA bases these updates on real-world data from thousands of patients, clinical trials, and post-market studies-not rumors or anecdotal reports. They review evidence from the FDA Adverse Event Reporting System (FAERS), which collects over 2 million reports annually. These are the most reliable safety updates available to the public.
What if I don’t understand the language in the "For Patients" section?
The FDA is required to write patient sections at an 8th-grade reading level. If it still feels confusing, ask your pharmacist or doctor to explain it. Many pharmacies now offer free consultations. You can also request a plain-language summary-these are now available for high-risk drugs in both English and Spanish on the FDA website.
Are these communications only for U.S. residents?
The FDA’s communications apply to drugs sold in the United States. If you’re outside the U.S., your country’s health agency (like the MHRA in the UK or EMA in Europe) may issue different alerts. But if you’re taking a U.S.-approved drug-even abroad-you should still check FDA updates, because many global health professionals use them as a reference.







2 Comments
I started signing up for FDA alerts after my mom had a bad reaction to her blood pressure med. Turns out there was a communication six months prior about interactions with grapefruit juice. She never read the label, and her doctor didn’t mention it. Now I get alerts for all her meds. Took five minutes to sign up. Could’ve saved her a hospital trip.
Don’t wait until something goes wrong. Set it and forget it.
As someone who works in regulatory affairs, I appreciate the clarity of this post. However, I must emphasize that the FDA’s Sentinel Initiative is not merely an analytical tool-it’s a public health infrastructure built on real-time data aggregation from Medicare, Medicaid, and private insurers. The 60+ communications annually are the tip of the iceberg; behind each is a statistical signal detected across millions of patient records.
Most patients don’t realize these aren’t anecdotal-they’re evidence-based thresholds crossed. That’s why the plain-language summaries are so critical.