
When someone is diagnosed with multiple myeloma, the focus often turns to blood tests, chemotherapy, and survival rates. But for more than 80% of patients, the most painful and life-limiting problem isn’t the cancer itself - it’s what the cancer does to their bones. This isn’t just osteoporosis or aging. It’s a rapid, aggressive breakdown of bone structure that leads to fractures, severe pain, and even paralysis. And for decades, treatment has been stuck in a holding pattern: slow-acting drugs that stop further damage but don’t fix what’s already broken.
How Myeloma Turns Bones Into Swiss Cheese
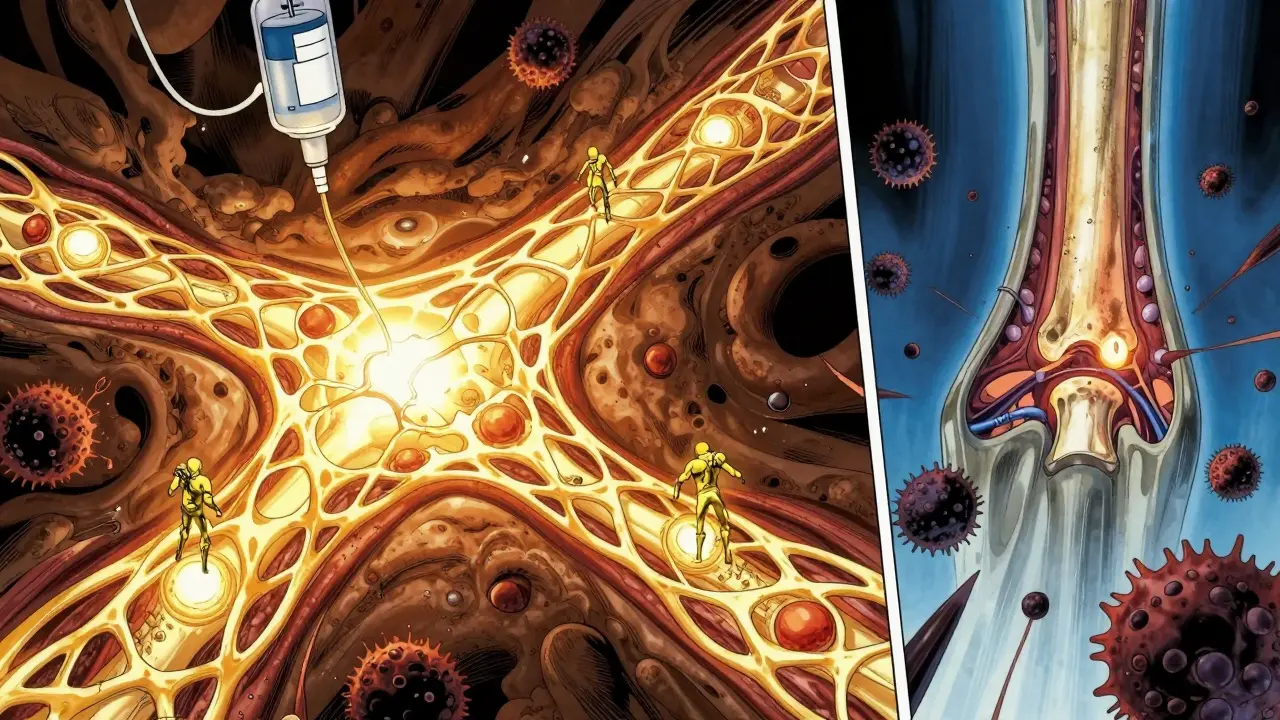
Multiple myeloma starts when abnormal plasma cells multiply in the bone marrow. These cells don’t just crowd out healthy blood cells - they hijack the body’s natural bone repair system. Normally, your bones are constantly being broken down and rebuilt in a balanced process. Osteoclasts chew away old bone; osteoblasts lay down new bone. In myeloma, this balance shatters.Myeloma cells pump out signals that tell osteoclasts to go into overdrive. At the same time, they shut down osteoblasts - the cells that build bone. The result? Holes in the bone that look like they’ve been punched out on X-rays. These aren’t random. They cluster where myeloma cells are most active. One study found patients with high levels of a protein called DKK1 had more than three times the number of bone lesions compared to those with lower levels. Another key player is sclerostin, a protein that blocks bone formation. In myeloma patients, sclerostin levels average nearly 50% higher than in healthy people.
This isn’t just a side effect - it’s a cycle. Every time a bone is destroyed, it releases growth factors that feed the myeloma cells. More tumor growth means more bone destruction. It’s a loop that keeps getting worse unless something breaks it.
What Happens When Bones Start to Fail
The consequences are brutal. About 30% of patients suffer pathological fractures - breaks that happen from something as simple as coughing or stepping off a curb. Spinal cord compression affects 5 to 10% of patients, sometimes leading to permanent nerve damage. And when bones break down too fast, calcium floods into the bloodstream, causing hypercalcemia - which can lead to confusion, kidney failure, or even coma.These aren’t rare events. Bone complications are the second most common reason myeloma patients end up in the hospital, after infections. On average, each hospital stay for a bone issue lasts over eight days. And even when patients survive, many live with chronic pain. A Reddit thread from early 2023 with nearly 150 patient comments showed that 68% still had bone pain despite being on standard treatment. Many also dealt with medication side effects: jawbone death (osteonecrosis), kidney damage from IV drugs, or sudden drops in calcium levels.
Current Treatments: Stopping the Bleeding, Not Healing the Wound
For years, the only tools doctors had were bisphosphonates - drugs like zoledronic acid and pamidronate. These are given monthly through an IV and work by killing off overactive osteoclasts. They reduce bone complications by about 15-18% compared to no treatment. But they don’t rebuild bone. They just slow the destruction.Then came denosumab - a drug that blocks a specific signal (RANKL) that tells osteoclasts to activate. It’s given as a monthly shot under the skin, which many patients prefer over IV infusions. In one Mayo Clinic study, 74% of patients chose denosumab over IV bisphosphonates because of convenience. But it’s expensive - about $1,800 per dose versus $150 for generic zoledronic acid. And while it’s effective at preventing fractures, it doesn’t reverse existing damage.
Both drugs carry risks. About 22% of patients on bisphosphonates need dose adjustments because of kidney problems. And around 42% of patients on either drug develop osteonecrosis of the jaw - a painful condition where the jawbone starts to die. That’s why dental checkups are now required before starting treatment.

The New Wave: Drugs That Actually Rebuild Bone
The real game-changer isn’t just stopping bone loss - it’s making bones grow back. That’s where the novel agents come in.One of the most promising is romosozumab, an antibody that blocks sclerostin. In a 2021 trial with 49 myeloma patients, those on romosozumab saw a 53% increase in bone density in the spine after just one year. Pain scores dropped by 35%. It’s not just slowing damage - it’s healing it. Another anti-sclerostin drug, blosozumab, showed a 47% drop in bone breakdown markers in a 2019 study.
Then there are drugs targeting DKK1. DKN-01, a DKK1 inhibitor, reduced bone resorption markers by 38% in a 2020 trial with 32 patients. And drugs aimed at the Notch pathway - like nirogacestat - cut osteolytic lesions by 62% in animal models. These aren’t just lab results. They’re signals that the bone marrow environment can be reprogrammed.
But here’s the catch: none of these drugs have yet proven they extend life. That’s the big question doctors are still trying to answer. As one expert put it, “We can fix the bone, but does that mean the patient lives longer?” Until we know which patients will benefit most, these drugs remain mostly in clinical trials.
Who Gets These New Drugs - And Why Not Everyone
Right now, romosozumab and DKN-01 are still in phase II or III trials. They’re not approved for routine use. Even when they are, access won’t be equal. In the U.S., denosumab is used in 78% of cases. In Europe, it’s only 42%. In Asia, bisphosphonates still dominate at 89%. Cost, reimbursement rules, and healthcare infrastructure all play a role.And monitoring these new drugs isn’t simple. Romosozumab can cause serious drops in calcium - so patients need monthly blood tests. Gamma-secretase inhibitors cause rashes in nearly 7 out of 10 patients. This means care has to be coordinated between hematologists, endocrinologists, and sometimes dermatologists or dentists. Many clinics aren’t set up for that.
What’s Next? Healing Bones, Not Just Protecting Them
The future isn’t just about more drugs - it’s about smarter use of them. Researchers are now testing combinations: a bone-building drug plus a tumor-targeting therapy. There are also RNA-based treatments in development, like Alnylam’s ALN-DKK1, which can silence the gene that produces DKK1 - cutting its levels by 65% in early tests.And the goal is shifting. No longer is it enough to prevent fractures. Experts now want to heal them. The FDA has approved a new, gentler version of zoledronic acid (Zometa-LD) with less kidney risk. A major phase III trial called BONE-HEAL is now recruiting 450 patients to test romosozumab’s ability to reverse bone damage. If it works, it could change everything.
By 2030, experts predict we’ll be able to heal myeloma bone lesions - not just stop them from getting worse. That means fewer hospital stays, less pain, and better quality of life. But we’re not there yet. The challenge now is making sure these advances reach everyone who needs them - not just those in big cities or wealthy countries.
What Patients Should Know Right Now
If you or someone you know has multiple myeloma:- Ask for a full bone scan - a whole-body low-dose CT or PET-CT - at diagnosis. Don’t settle for just an X-ray.
- Get a dental checkup before starting any bone-targeting therapy. Preventing jawbone damage is easier than treating it.
- Track your calcium levels. If you’re on denosumab or a new trial drug, low calcium can sneak up on you.
- Ask about clinical trials. Many novel agents are only available through research studies.
- Use trusted resources like the International Myeloma Foundation’s Bone Disease Management Guide. It’s been downloaded over 18,000 times for a reason.
The story of myeloma bone disease is changing. For decades, it was seen as an unavoidable side effect. Now, we know it’s a target. And targeting it - with the right drugs, at the right time - might be the key to not just surviving myeloma, but living well with it.
Is bone damage from multiple myeloma reversible?
Traditional treatments like bisphosphonates and denosumab stop further bone loss but don’t rebuild bone. However, new drugs in clinical trials - such as romosozumab and anti-DKK1 therapies - have shown the ability to increase bone density and reduce lesions. Early results suggest bone healing is possible, but these treatments are not yet widely available outside of research studies.
Why do myeloma patients get fractures so easily?
Myeloma cells disrupt the normal balance between bone breakdown and rebuilding. They overactivate osteoclasts (cells that destroy bone) and suppress osteoblasts (cells that build bone). This creates weak, porous areas called osteolytic lesions. These areas are so fragile that even minor stress - like lifting a grocery bag or sneezing - can cause a fracture.
What’s the difference between zoledronic acid and denosumab?
Both drugs reduce bone complications, but they work differently. Zoledronic acid is a bisphosphonate given as a monthly IV infusion. It kills osteoclasts directly. Denosumab is a monthly injection under the skin that blocks RANKL, a protein that activates osteoclasts. Many patients prefer denosumab because it’s easier to administer and doesn’t affect the kidneys as much - but it’s significantly more expensive.
Can I avoid bone problems if I’m diagnosed with myeloma?
You can’t always prevent them, but you can reduce the risk significantly. Start bone-protecting therapy right after diagnosis, get regular imaging, maintain vitamin D and calcium levels, avoid smoking, and get a dental evaluation before starting treatment. Early intervention is the best defense against fractures and spinal cord compression.
Are there any new drugs for myeloma bone disease coming soon?
Yes. Romosozumab is in a large phase III trial called BONE-HEAL, with results expected in 2026. Anti-DKK1 drugs like DKN-01 and RNA-based therapies targeting bone signals are also advancing. Several bispecific antibodies that attack both myeloma cells and bone-damaging pathways are in early trials. These could become standard within the next 3-5 years, especially if they show survival benefits.



13 Comments