
When someone says they feel like they might die, and they’re not exaggerating - that’s often the first real sign of sepsis. It’s not just a bad infection. It’s your body’s own defenses turning against you, triggering a chain reaction that can shut down organs and kill you within hours. Every minute counts. In the UK, someone dies of sepsis every three minutes. But here’s the truth: if caught early, most people survive. The difference isn’t luck - it’s recognition and speed.
What Sepsis Really Is (And Why It’s Not Just an Infection)
Sepsis isn’t the infection itself. It’s what happens when your immune system goes into overdrive trying to fight off an infection - whether it’s pneumonia, a urinary tract infection, a cut that got infected, or even a tooth abscess. Instead of protecting you, your body starts damaging your own tissues and organs. This is called organ dysfunction. The key marker? A rise of two or more points on the SOFA score - a clinical tool doctors use to measure how badly your organs are failing. That jump means your risk of death goes up by 10% for every point. That’s why sepsis is often called a silent killer. You might think you’ve got the flu. But your kidneys, lungs, or heart are already struggling.The Six Signs You Can’t Ignore (It’s Not Just Fever)
Most people expect sepsis to mean high fever. But that’s only part of the story. The real danger lies in the subtle, terrifying changes that don’t show up on a thermometer.- Slurred speech or confusion - This happens in nearly half of adult cases. You might not realize you’re acting strangely. A family member might notice you can’t remember your own address or keep track of a simple conversation.
- Extreme pain or discomfort - Patients describe this as the worst pain they’ve ever felt - worse than childbirth, worse than a broken bone. It’s not localized. It’s full-body, deep, and unrelenting.
- Pale, blotchy, or blue-tinged skin - Especially around the lips, fingers, or toes. This isn’t just looking pale. It’s a grayish, mottled, or bluish discoloration that doesn’t improve with warmth. In children, it’s often the first visible clue.
- Severe breathing difficulty - Breathing faster than 22 breaths per minute. You’re not just out of breath from walking. You’re gasping, even at rest. Your body is begging for oxygen because your lungs are failing.
- Extreme sleepiness or difficulty waking - You can’t stay awake. You don’t respond when called. This isn’t tiredness. It’s neurological shutdown.
- ‘I feel like I might die’ - This isn’t anxiety. It’s a gut feeling reported by 78% of patients before they’re diagnosed. If someone says this - believe them. Call 999 immediately.
For babies under three months, watch for: no wet diaper in over 12 hours, extreme lethargy (not just fussy - unresponsive), and a temperature above 38°C or below 36°C. Don’t wait for a rash. Only 15% of sepsis cases have a non-fading rash - but if you see one, it’s a medical emergency.
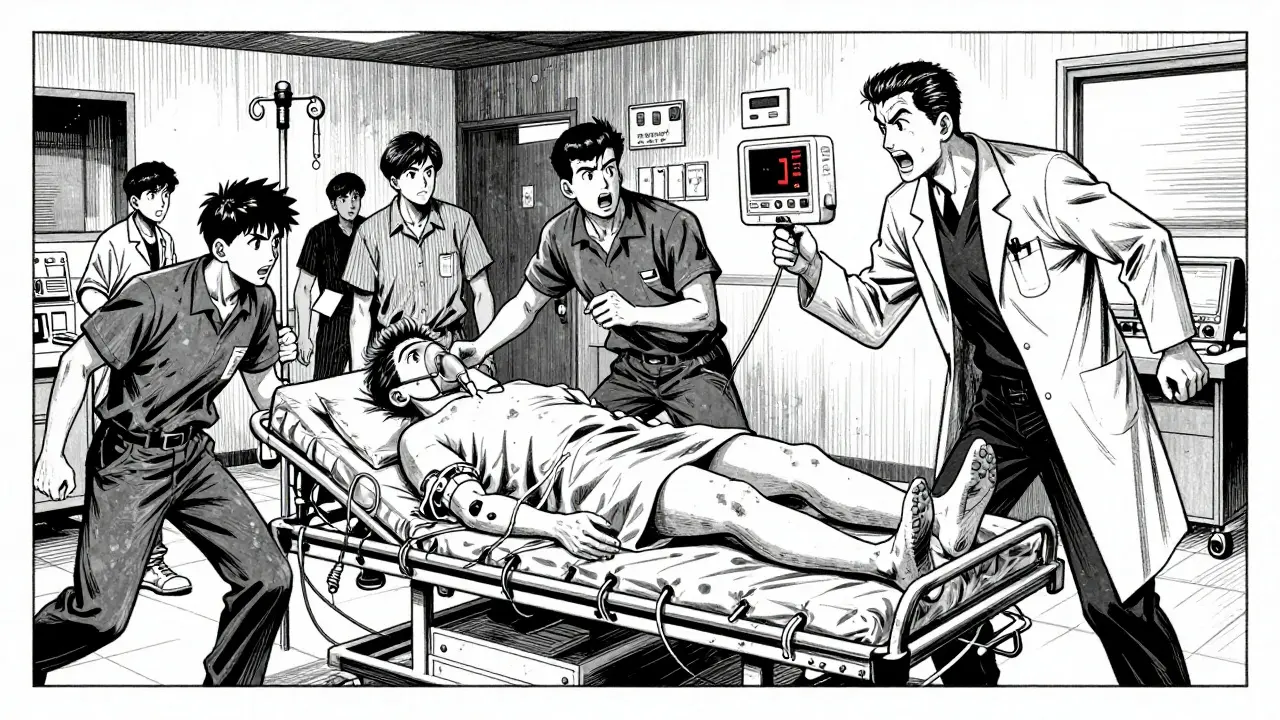
What Happens When You Get to the Hospital
Once you arrive at the ER, time becomes the enemy. The clock starts ticking from the moment you walk in. In the UK, hospitals follow the ‘Sepsis Six’ protocol - six critical steps that must be completed within the first hour.- Broad-spectrum antibiotics - Given intravenously immediately. Common choices are piperacillin-tazobactam or meropenem. Delaying antibiotics by even one hour increases your chance of dying by 7.6%.
- Blood cultures - Taken before antibiotics, but not after. These help identify the exact bacteria causing the infection so treatment can be targeted later.
- IV fluids - At least 30 mL per kilogram of body weight, given within three hours. This isn’t just hydration. It’s about keeping your blood pressure up so your organs keep getting oxygen.
- Serum lactate test - A level above 4 mmol/L means your body is in severe distress. Your cells aren’t getting enough oxygen, so they’re switching to inefficient energy production. This is a red flag for septic shock.
- Oxygen therapy - If your oxygen saturation is below 94%, you’ll get oxygen through a mask or nasal cannula. The goal? Keep it between 94% and 98%. Too much oxygen can be harmful too.
- Urine output monitoring - Doctors track how much you pee. Less than 0.5 mL per kilogram per hour means your kidneys are failing. This triggers more aggressive treatment.
Hospitals that hit 90% compliance with this one-hour bundle cut sepsis deaths from nearly 27% to under 20%. That’s thousands of lives saved every year.
What Happens If It Gets Worse (Septic Shock)
If your blood pressure stays dangerously low even after fluids, you’ve entered septic shock. This is where things get critical. At this stage, your body needs stronger support.- Norepinephrine - This is the first-line drug to raise blood pressure. It’s given through an IV and slowly adjusted until your mean arterial pressure hits 65 mmHg - the minimum needed to keep organs alive.
- Source control - If there’s an abscess, infected IV line, or ruptured appendix, doctors will remove or drain it within 6 to 12 hours. No antibiotic can fix an ongoing source of infection.
- Corticosteroids - If you need multiple drugs to keep your blood pressure up, you might get hydrocortisone. It doesn’t lower your overall death risk, but it shortens how long you’re in shock by about a day and reduces your ICU stay.
Recent advances are helping. The FDA-approved Accelerate PhenoTest BC Kit can identify bacteria and their antibiotic resistance in just 90 minutes - down from two to three days. That means you get the right antibiotic faster, not just any antibiotic.
Surviving Sepsis - The Long Road After the Emergency
Getting through the first 48 hours doesn’t mean you’re out of the woods. One in three survivors still ends up back in the hospital within a month - often for another infection, breathing problems, or heart issues.- 60% still feel exhausted six months later.
- 45% struggle with shortness of breath during normal activities.
- 38% have chronic muscle and joint pain.
- 32% have trouble walking or climbing stairs.
- 29% can’t sleep properly.
This is called Post-Sepsis Syndrome. It’s not just physical. Many survivors report memory loss, trouble concentrating, and depression. The good news? Starting rehab within 72 hours of ICU admission cuts long-term disability by 22%. That means gentle movement, breathing exercises, and physical therapy - even while still in hospital.

Why Speed Saves Lives - And Why It’s Still Not Good Enough
The science is clear: every hour without antibiotics raises your risk of death. Yet, in the UK and US, over half of survivors waited more than three hours to get treatment. Nearly one in four waited over six hours. Why? Because sepsis looks like the flu. Because people don’t know the signs. Because doctors miss it in busy ERs.But things are changing. Hospitals that use automated sepsis alert systems - triggered by vital signs like high heart rate, low blood pressure, or high lactate - reduce time to antibiotics by almost an hour. That’s a 5.3% drop in death rates.
Still, disparities remain. Black patients in the US wait 18% longer for antibiotics and have 23% higher death rates than white patients. This isn’t about biology - it’s about bias, access, and systemic gaps in care.
What You Can Do
You don’t need to be a doctor to save a life. Learn the signs. Trust your gut. If someone says, “I feel like I’m going to die,” don’t wait. Don’t call your GP. Don’t wait to see if it gets worse. Call 999. Say, “I think this is sepsis.” Use the word. It gets people moving.Keep the Sepsis Six in mind - especially if someone is sick with an infection and starts acting wrong. Fever? Check. But confusion? Pale skin? Can’t wake up? That’s not the flu. That’s sepsis. And time is everything.
Can sepsis be caught early enough to avoid hospitalization?
No. Once sepsis develops, hospital care is required. Even mild cases need IV antibiotics and close monitoring. You can’t treat sepsis at home. Delaying hospital care increases the risk of death dramatically. If you suspect sepsis, go straight to the emergency department - don’t wait.
Is sepsis contagious?
No. Sepsis itself is not contagious. But the infection that triggers it - like pneumonia, a UTI, or a skin infection - can be. You can catch the bacteria or virus that might lead to sepsis, but you won’t catch sepsis directly from someone else.
What’s the difference between sepsis and septic shock?
Sepsis is organ dysfunction caused by infection. Septic shock is a more severe form where your blood pressure stays dangerously low even after fluids are given. You need strong medications called vasopressors to keep your organs alive. Septic shock has a much higher death rate - up to 40% in some cases.
Can antibiotics alone cure sepsis?
Not always. Antibiotics are essential, but they’re only one part of treatment. You also need fluids to maintain blood pressure, oxygen if your levels are low, and sometimes surgery to remove the source of infection - like draining an abscess or removing an infected device. Without these, antibiotics won’t be enough.
How long does it take to recover from sepsis?
Recovery varies. Some people feel better in weeks. Others take months or even years. Many survivors deal with long-term fatigue, muscle weakness, and cognitive issues. Early rehab in the hospital improves outcomes. Full recovery often requires physical therapy, counseling, and ongoing medical follow-up.
Are there new treatments for sepsis on the horizon?
Yes. New rapid diagnostic tests can identify the exact bacteria and antibiotic resistance in under two hours, allowing faster, targeted treatment. Researchers are testing drugs that modulate the immune response to prevent the body from attacking itself. One promising drug, interferon gamma, reduced organ failure days by 15% in early trials. But the biggest breakthrough so far is better systems - faster alerts, better training, and public awareness.
Next Steps: What to Do If You’re Worried
If you’re caring for someone who’s sick and starting to act differently - confused, pale, breathing hard, unresponsive - act now. Don’t wait for a fever. Don’t wait for a rash. Don’t wait to see if they get better. Call 999. Say, “I think this is sepsis.”If you’ve survived sepsis, don’t ignore lingering symptoms. Fatigue, memory problems, or trouble walking aren’t just ‘normal’ after being sick. They’re signs you need follow-up care. Ask your GP for a referral to a post-sepsis clinic if one exists in your area.
Sepsis doesn’t care who you are. But speed, knowledge, and action - yours - can make all the difference.







10 Comments