
If your child swallows the wrong medication, time is everything. Every second counts. The difference between a quick recovery and a life-threatening emergency often comes down to what you do in the first five minutes. There’s no time to panic, no time to Google, and no time to wait and see. You need clear, proven steps - and you need them now.
Call Poison Control Immediately - Before Anything Else
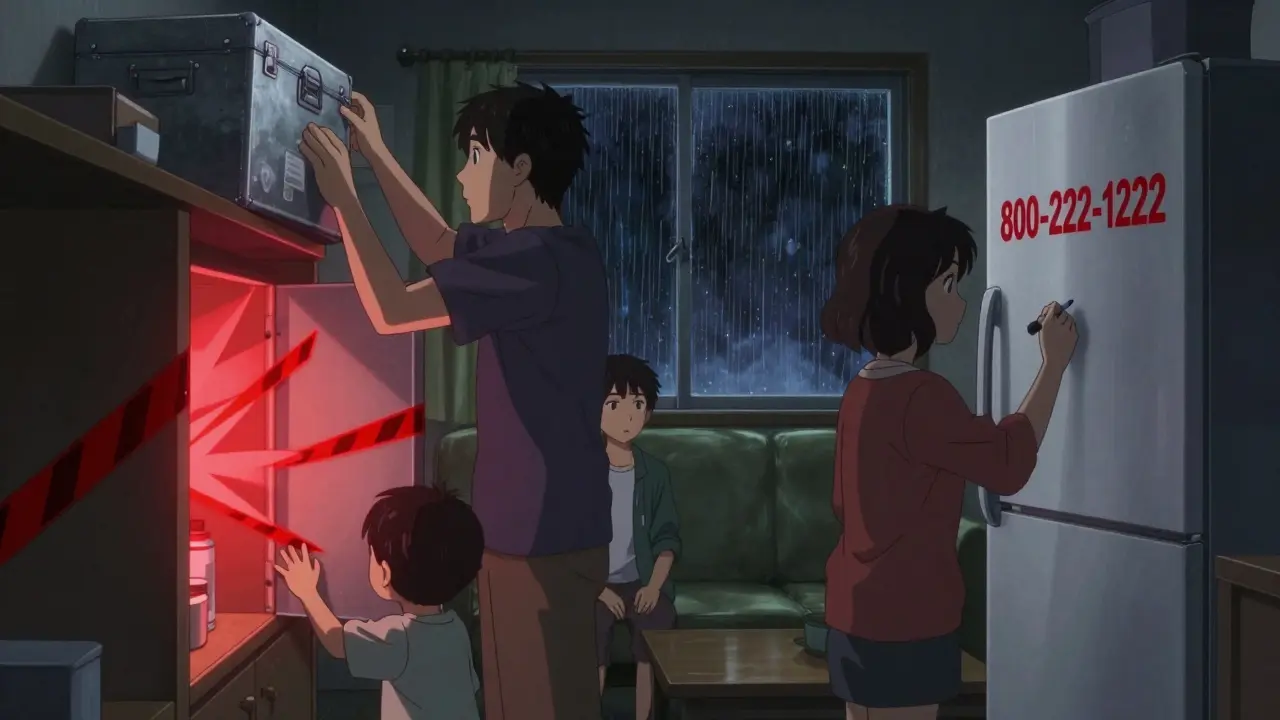
The very first thing you must do is call Poison Control. In the U.S., dial 800-222-1222. In the UK, call 111 or go to NHS 111 online. Don’t wait to see if your child looks sick. Don’t try to figure out what they swallowed first. Just call. Poison Control specialists are trained to handle these emergencies in real time. They’ll ask you for details - the medicine name, how much was taken, your child’s age and weight - and then give you exact instructions based on that specific drug.Most parents don’t know this number. A 2022 survey found only 61% of caregivers could correctly recall the Poison Help line. That’s why the American Association of Poison Control Centers launched its "Know the Number" campaign in January 2023. Save it in your phone right now. Put it on the fridge. Tell every babysitter, grandparent, and family member who watches your child.
Do not delay. Studies show that when families contact Poison Control within minutes of ingestion, hospitalization rates drop by 43%. One mom in Ohio saved her 2-year-old after he swallowed three chewable antihistamines. She called immediately. Poison Control told her to watch for drowsiness and check his breathing every 15 minutes. He didn’t need to go to the ER. Another dad waited 45 minutes to find the pill bottle before calling. His child ended up in the hospital for 36 hours after swallowing a single blood pressure pill.
Remove Any Remaining Medication - But Don’t Induce Vomiting
While you’re on the phone with Poison Control, quickly check your child’s mouth. If you see any pills, liquid, or patches, gently remove them with your fingers. Don’t use tools. Don’t stick your fingers deep. Just get out what’s visible.Here’s what you must NOT do: do not make your child throw up. For decades, parents were told to use syrup of ipecac. That advice is outdated - and dangerous. Since 2004, no major medical group recommends it. Why? Because vomiting doesn’t reliably remove the poison. Instead, it can cause the child to inhale stomach contents into their lungs, leading to pneumonia. Studies show it helps in less than 1% of cases but causes serious harm in 7% of attempts.
If the medication was a patch - like fentanyl or nicotine - check the child’s skin and even the roof of their mouth. Patches can stick to the tongue or gums when sucked on. Peel them off carefully, using gloves if you have them. Wash your hands right after.
Watch for These Life-Threatening Symptoms
Not all poisonings look the same. Some kids seem fine at first. Others crash fast. Know the red flags that mean you need to call 911 right now:- Difficulty breathing or stopped breathing
- Loss of consciousness or extreme drowsiness that won’t wake them
- Seizures or uncontrolled shaking
- Pupils that are unusually large or tiny
- Heartbeat that’s too slow (under 50 beats per minute) or too fast
- Bluish lips or skin
Pain medications like acetaminophen (Tylenol) are the leading cause of poisoning deaths in young children. A single adult tablet can cause liver failure. Blood pressure pills like amlodipine can drop a child’s blood pressure to dangerous levels within 30 minutes. Antidepressants and heart medications can trigger abnormal rhythms. Even common cold medicines can cause seizures if too much is taken.
If you see any of these signs, don’t wait for Poison Control to tell you what to do. Call 911 immediately. While you wait, keep your child awake and sitting up if possible. Don’t give them anything to eat or drink unless instructed.

What Happens at the Hospital?
If you’re sent to the ER, doctors will follow a strict protocol. They’ll want to know exactly what was swallowed, when, and how much. Bring the bottle - even if it’s empty. The label has critical info.Most kids will be monitored for at least 12 hours. If it’s a heart or diabetes medication, they’ll be hooked up to a heart monitor. Blood sugar will be checked every 30 minutes if a sulfonylurea (like glipizide) was involved - low blood sugar can sneak up without symptoms.
Common treatments include:
- Activated charcoal - given within one hour to absorb the poison in the gut. It’s not used for all drugs, like cleaning products or petroleum-based substances.
- Naloxone - if opioids (like hydrocodone or oxycodone) were taken. This can reverse breathing problems in seconds.
- Octreotide - for insulin or sulfonylurea overdoses to prevent dangerous drops in blood sugar.
- Sodium bicarbonate - for tricyclic antidepressant overdoses to protect the heart.
There’s no one-size-fits-all fix. Treatment depends on the drug, the dose, and how long it’s been since ingestion. That’s why calling Poison Control first is so vital - they guide you to the right care.
Why Prevention Is the Only Real Solution
The best way to handle a medication emergency? Avoid it altogether.Lock up all medicines. Not just in a cabinet - use a locked box or childproof container. The CDC found homes with locked storage have 85% fewer accidental ingestions. Liquid medications now come with flow restrictors that cut the amount a child can swallow by 58%. Make sure yours has one.
Never leave pills on a nightstand, in a purse, or on the counter. Even if you think you’re just going to be gone for a minute. Kids are fast. They climb. They explore. A single pill can be fatal.
Smart pill bottles like Hero Health’s system can alert you if a bottle is opened. They cost about $90 a month, but they’ve cut accidental access by 73% in studies. Most families can’t afford them - but you don’t need tech to stay safe. A simple lock on a high cabinet works just as well.
Also, never refer to medicine as candy. Don’t say, "This will make you feel better, like a treat." That confuses kids. Teach them early: "Medicine is not food. Only adults give medicine."
What to Do After the Emergency
Even if your child seems fine after a small ingestion, watch them closely for 24 hours. Some drugs cause delayed effects. Acetaminophen, for example, can damage the liver over 2-3 days. Call your pediatrician for follow-up advice.Take this as a wake-up call. Re-evaluate your home. Are all medicines locked? Are visitors aware? Are old prescriptions still lying around? Get rid of expired meds at a pharmacy drop box. Don’t flush them - it pollutes water systems.
Share this information. Talk to other parents. Post the Poison Control number on your fridge. Teach your older kids what to do if a sibling swallows something. Knowledge saves lives.
What should I do if my child swallows a pill I didn’t know they could reach?
Call Poison Control immediately at 800-222-1222. Don’t wait for symptoms. Don’t try to make them vomit. Remove any visible pills from their mouth. Have the medicine bottle ready when you call. Follow their instructions exactly - they may tell you to watch at home or go to the ER.
Can I use syrup of ipecac to make my child throw up?
No. Syrup of ipecac is no longer recommended by any major medical organization. It doesn’t reliably remove poison and can cause serious harm, including aspiration pneumonia. The American Academy of Pediatrics removed it from guidelines in 2004. Never use it.
How quickly can a child get sick after swallowing medicine?
It depends on the drug. Some, like heart or blood pressure pills, can cause dangerous drops in blood pressure or heart rate within 15-30 minutes. Others, like acetaminophen, may not show symptoms for hours or even days. Always assume the worst and act fast. Don’t wait for signs.
Is it safe to give my child milk or water after they swallow medicine?
Only if Poison Control or a doctor tells you to. Some drugs react badly with food or liquids. For example, giving milk after an iron overdose can slow absorption and delay treatment. Wait for expert advice before giving anything by mouth.
What if I don’t know what my child swallowed?
Call Poison Control anyway. They’ve handled millions of cases like this. Tell them everything you saw - the color of the pill, the shape, if there was liquid, any packaging left behind. Even partial info can help them guide you. They’ll likely advise you to go to the ER for monitoring.
Are child-resistant caps really effective?
They help - but they’re not foolproof. Most kids under 3 can open them in under 5 minutes. That’s why locking medicines in a high, locked cabinet is still the best protection. Child-resistant caps are a backup, not a solution.
Can I use the webPOISONCONTROL tool instead of calling?
It’s a good tool for non-emergencies - like if you’re unsure whether a small dose is dangerous. But if your child is showing symptoms or swallowed a large amount, call 800-222-1222. The online tool has 94% accuracy, but live specialists can adapt instantly to your child’s condition and give real-time guidance.
Next Steps: Protect Your Home Today
Right now, do this:- Find every medicine in your house - including vitamins, supplements, and old prescriptions.
- Put them all in a locked box or high cabinet with a childproof latch.
- Save 800-222-1222 in your phone and write it on the fridge.
- Teach your kids: "Medicine is not candy. Only grown-ups give medicine."
- Check your child’s room, the car, and your purse - those are common places for accidental access.
Accidents happen. But with the right knowledge and preparation, you can turn a potential tragedy into a managed event - or better yet, prevent it entirely.


13 Comments
Yo, this post is legit life-saving stuff. I used to think ipecac was the move until my cousin’s kid swallowed half a bottle of ibuprofen and the ER doc nearly yelled at her for trying it. Don’t be that person. Save the number. Lock it up. Done.
so i just saved 800-222-1222 to my phone under ‘emergancy’ lol. also put it on the fridge next to the pizza menu. my 3yo thinks the fridge is a treasure chest so… yknow. better safe than sorry.
call poison control first? revolutionary. next youll tell us not to lick batteries
While the guidance is accurate and well-intentioned, I must note that the reliance on Poison Control as a primary intervention assumes consistent access to telecommunication infrastructure, which is not universally available. In rural or underserved communities, response latency may negate the time-sensitive advantage described. Additionally, the efficacy of activated charcoal is highly pharmacokinetic-dependent - its utility diminishes sharply beyond the 60-minute window, yet the post implies broad applicability. A more nuanced discussion of drug-specific toxidromes would elevate the utility of this resource.
Just read this after my niece swallowed a melatonin gummy. We called Poison Control. They said watch her sleep it off. She woke up fine. This post saved us from a panic drive to the ER. Thanks.
Let’s deconstruct the neoliberal myth of the ‘responsible parent’ here - the burden of preventing pediatric ingestion is disproportionately placed on caregivers, particularly mothers, while pharmaceutical companies peddle child-unfriendly packaging with patent-protected child-resistant caps that are, statistically, laughably ineffective. We are not failing because we’re negligent - we’re failing because the system is designed to commodify safety while outsourcing liability to the domestic sphere. Lock your meds? Sure. But ask why the FDA still allows 100-count bottles of acetaminophen to be sold like candy at gas stations. The real poison isn’t the pill - it’s the capitalism that profits from your fear.
my sister’s kid got into her blood pressure meds and she waited 20 minutes to call because she was ‘trying to figure out if it was bad’ and now the kid has brain damage and she won’t talk to anyone and i just cried for 45 minutes and i’m not okay and nobody told me this stuff before and why is this not taught in school and why are we still letting people have pills lying around like it’s 1998
ok but what if the poison control person is racist?? i heard this lady in texas got told to ‘just watch her’ and the kid died and now she’s in a coma and i’m not even kidding i saw it on tiktok and the comments were wild and i don’t trust ANY system anymore 😭
you think locking meds up is enough? what about the grandma who brings her ‘special vitamins’ from her church group? what about the cousin’s vape pen that looks like a highlighter? what about the unmarked bottle in the bathroom cabinet labeled ‘for migraines’ that’s actually fentanyl patches? this post is cute but it’s a Band-Aid on a hemorrhage. we’re all one careless moment away from a funeral and no amount of fridge stickers will fix that.
In many cultures, including those in South Asia and parts of Africa, the concept of storing pharmaceuticals in locked containers is culturally alien. Medications are often kept in accessible locations due to economic necessity, lack of storage infrastructure, or traditional beliefs regarding healing. While the recommendations here are medically sound, they may inadvertently stigmatize caregivers in resource-constrained environments. A culturally adaptive approach - such as community-based education and low-cost pill-dispensing pouches - may yield more sustainable outcomes.
I’m a paramedic. I’ve seen this too many times. The parents who call immediately? Their kids walk out. The ones who wait? They don’t. I don’t say this to scare you - I say it because I’ve held the hand of a 4-year-old who stopped breathing because someone thought, ‘Maybe it’s not that bad.’ Don’t be that person. Call. Now. Then breathe.
thank you for this. i just found my 5yo with my antidepressants in her mouth. i called poison control. they said give her water and wait. i’m shaking but i’m so glad i didn’t try to make her throw up. i’m putting the meds in a lockbox tonight. i’m so scared.
Lock it. Save the number. Teach your kids. Do it now. Not tomorrow. Not when you’re ‘less busy.’ This isn’t advice - it’s a survival protocol. Your child’s life doesn’t come with a second chance.