
If you're taking a blood thinner-whether it's warfarin, Eliquis, Xarelto, or Pradaxa-you know it's meant to keep you safe from clots. But what happens when you take too much? Or when a loved one accidentally takes a double dose? The truth is, blood thinner overdose doesn't always come with a warning. One minute you feel fine. The next, you're bleeding internally with no visible sign. And every hour counts.
What Happens When You Take Too Much?
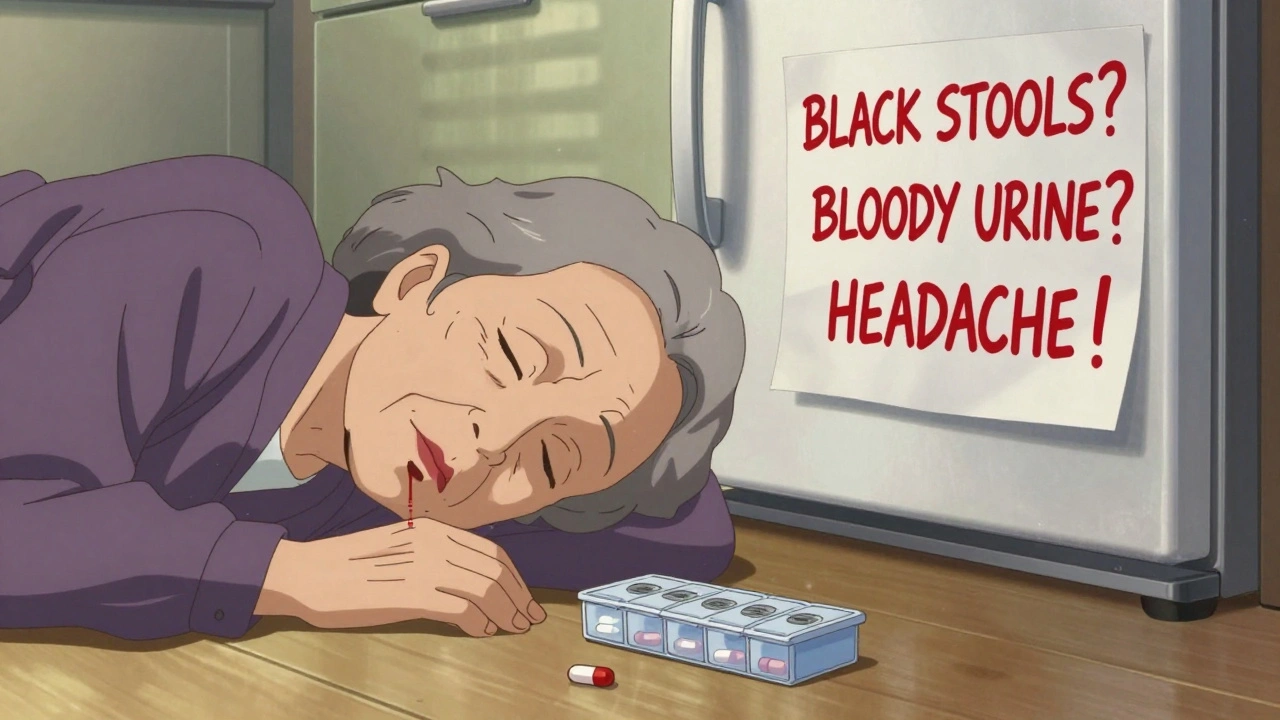
Blood thinners work by slowing down your body’s ability to form clots. That’s good when you have atrial fibrillation or a history of DVT. But if your dose is too high, your blood can’t clot at all. Even a small bump can turn into a dangerous bleed inside your body. The most dangerous part? You might not feel it until it’s too late. Warfarin, the oldest blood thinner, takes days to fully kick in. Your INR (a blood test that measures clotting time) might spike slowly-sometimes 12 to 24 hours after an overdose. But newer drugs like apixaban or rivaroxaban work fast. An accidental double dose can send your clotting time through the roof within hours. And unlike warfarin, there’s no easy way to check your levels at home with these. Here’s what an overdose looks like in real life:- Bloody or black, tarry stools
- Spitting up or coughing up blood
- Pink, red, or dark brown urine
- Vomiting material that looks like coffee grounds
- Unexplained bruising-especially large, spreading bruises
- Small red or purple dots under the skin (petechiae)
- Heavy menstrual bleeding that’s new or worse than usual
- Severe headache, dizziness, weakness, or confusion
- Sharp pain in your back, belly, or chest
These aren’t side effects. These are red flags. And they mean your body is bleeding inside-possibly into your brain, stomach, or kidneys.
When to Call 999 (Not Wait)
Too many people delay. They think, “It’s just a nosebleed.” Or, “I’ll wait until morning.” But when you’re on a blood thinner, waiting even a few hours can be deadly. The NHS and Mayo Clinic both say: if bleeding from a cut, nose, or gum doesn’t stop after 10 minutes of direct pressure-call emergency services. Same if you see any of the symptoms above. Even if you feel fine. A 2022 study by the National Blood Clot Alliance found that patients who got help within two hours of noticing bleeding had a 97% survival rate. Those who waited six hours or more? Only 76% made it. One Reddit user, u/WarfarinWarrior, shared how he ignored dark stools for three days, thinking it was food. By the time he reached the ER, his hemoglobin had dropped to 6.2 g/dL (normal is 12-16). His INR was 8.7. He needed a blood transfusion and intensive care. Don’t be that person. If you suspect an overdose-call now. Don’t text. Don’t ask a friend. Call 999.What to Do Right Now
While you wait for help, here’s what you must do:- Do NOT take another dose. Even if you think you missed one. Overdose is not a missed dose-it’s too much.
- Write down what you took. Name of the drug, how much, and when you took it. If you’re alone, leave a note on the counter. Emergency teams need this fast.
- Don’t take ibuprofen, aspirin, or naproxen. These make bleeding worse. Even a single tablet can push you over the edge.
- Lie down. Elevate any bleeding area above your heart if you can. This slows blood flow to the site.
- Apply firm pressure. For external bleeding, press hard for at least 10 minutes. Don’t peek. Let the blood clot.
And here’s the one thing you should NOT do: try to “wait it out.” There’s no home remedy. No herbal tea. No vitamin K you can swallow to fix it. Not yet.
What Happens at the Hospital?
Emergency teams don’t guess. They test. They check your INR. They look for signs of bleeding in your brain, gut, or kidneys. Then they act. If it’s warfarin and your INR is over 3.5, they’ll give you vitamin K-usually by mouth if you’re stable, or IV if you’re bleeding. But vitamin K takes hours to work. So if you’re actively bleeding, they’ll use something stronger: 4-factor Prothrombin Complex Concentrate (PCC). This is a concentrated mix of clotting factors that can reverse warfarin in minutes. For newer drugs like Eliquis or Xarelto, there are specific antidotes:- idarucizumab for Pradaxa (dabigatran)
- andexanet alfa for Eliquis and Xarelto (apixaban, rivaroxaban)
These cost thousands of pounds per dose-but they work fast. In under 15 minutes, they can restore your blood’s ability to clot. That’s why hospitals keep them on hand.
For very recent overdoses (within an hour), they might give you activated charcoal to stop the drug from absorbing. But after that? It’s too late. Your body already took it.
Who’s at Highest Risk?
It’s not just about how much you take. It’s about who you are. People over 65 are four times more likely to have a serious bleeding event on blood thinners. Why? Slower metabolism. Kidney issues. More meds. The HAS-BLED score-a tool doctors use-gives you one point each for:- Hypertension
- Abnormal kidney or liver function
- History of stroke
- Previous bleeding
- Unstable INR levels
- Age over 65
- Drinking alcohol or taking other drugs like NSAIDs
If your score is 3 or higher? You’re in the high-risk zone. That means you need more frequent checks. More education. And a clear plan for what to do if things go wrong.
How to Prevent This From Happening
Prevention beats emergency every time.- Use a pill organizer. Not just any one-get one with alarms or one that locks. Many people accidentally take double doses because they forget if they already took it.
- Keep a bleeding risk checklist. Tape it to your fridge. List the symptoms above. Check it daily.
- Get regular INR tests. If you’re on warfarin, you need them weekly at first. Once stable, maybe monthly. Don’t skip them.
- Use a home INR monitor. These portable devices cost £200-£300. Studies show they cut major bleeding by 34%. If you’re high-risk, ask your doctor if you qualify.
- Tell every doctor you see. Dentists, pharmacists, surgeons-they all need to know you’re on a blood thinner. Even a simple tooth extraction can turn dangerous.
- Never mix with NSAIDs. Ibuprofen, naproxen, even aspirin for headaches? Avoid them. Use paracetamol instead.
- Keep a list of your meds. Include dosages and times. Carry it in your wallet. Your phone’s notes app doesn’t help if you’re unconscious.

What’s Changing in 2025?
There’s new hope. Ciraparantag-a universal reversal agent-is in final trials. It can reverse all blood thinners in under 10 minutes. No need to know which drug you took. No waiting for PCC or antidotes. Just inject and clotting starts. The FDA approved it for emergency use in early 2025. Hospitals in the UK are starting to stock it. This could be the biggest advance since warfarin was invented in 1948. But until then? You still need to know the signs. You still need to act fast.Final Thought: This Isn’t Rare
In the UK, anticoagulant overdoses cause more emergency visits than insulin errors or opioid overdoses. The CDC says it’s the second most common serious medication error in people over 65. You’re not alone. But you are responsible-for your own safety, and for the people who care about you. If you take a blood thinner, you’re carrying a silent timer. You can’t see it. But it ticks every day. Don’t let it run out.Can you reverse a blood thinner overdose at home?
No. There is no safe or effective way to reverse a blood thinner overdose at home. Vitamin K helps with warfarin, but it takes hours to work and doesn’t stop active bleeding. If you suspect an overdose, call emergency services immediately. Do not wait, even if you feel fine.
What should I do if I accidentally take two doses of my blood thinner?
Do not take another dose. Call 999 or go to the nearest emergency department immediately. Even if you feel okay, your blood clotting levels could drop dangerously within hours. Bring the medication bottle with you so the medical team knows exactly what you took.
Is it safe to take paracetamol while on blood thinners?
Yes, paracetamol (acetaminophen) is generally safe to use with blood thinners for pain or fever. Avoid ibuprofen, naproxen, aspirin, or other NSAIDs-they increase bleeding risk. Always check with your pharmacist before taking any new medication, even over-the-counter ones.
How often should I get my INR checked if I’m on warfarin?
When you first start warfarin, you’ll need weekly checks. Once your dose is stable and your INR stays in the target range (usually 2.0-3.0), you may only need testing every 4-6 weeks. But if your INR fluctuates, you’re elderly, or you’re on other medications, you may need weekly tests for longer. Always follow your doctor’s advice.
Can I still drink alcohol while on blood thinners?
Moderate alcohol use (one drink per day) is usually okay, but heavy drinking is dangerous. Alcohol can interfere with how your liver processes warfarin, making your INR unstable. It also increases your risk of falls and injuries. If you drink regularly, tell your doctor-it affects your HAS-BLED score and your bleeding risk.
What are the signs of internal bleeding in the brain?
Signs include sudden severe headache, dizziness, confusion, trouble speaking, weakness on one side of the body, blurred vision, or loss of consciousness. Even a minor head injury can cause a bleed if you’re on a blood thinner. If you have any of these symptoms, call 999 immediately-even if you didn’t hit your head hard.
Do I need to carry an emergency card for my blood thinner?
Yes. Many UK hospitals recommend carrying a medical alert card or bracelet that lists your medication, dose, and emergency contact. Some pharmacies offer free cards. If you’re unconscious in an emergency, this information can save your life.







10 Comments
OMG I thought I was the only one who forgot if I took my pill and then doubled down 😭 my mom did this last year with warfarin and ended up in the ER with a GI bleed. Just got my new pill organizer with alarms last week-life saver. If you’re on these meds, get one. Seriously.
Stop scaremongering. Blood thinners are overprescribed. Most people don’t need them. I’ve seen 70-year-olds on Eliquis for ‘mild AFib’ who’ve never had a stroke. The real danger is the pharmaceutical industry pushing these drugs because they’re profitable. Vitamin K is free. Why not just eat more kale?
They’re lying about the antidotes. Andexanet alfa? That’s just a cover-up. The real reversal agent is already out there-Ciraparantag. But the FDA won’t approve it because Big Pharma doesn’t want you to have a universal fix. They profit off you needing different antidotes for each drug. Wake up. The system is rigged. Check the clinical trial records. They’re hiding data.
Why do they even make these drugs if they’re so dangerous? It’s not about health-it’s about control. The government wants old people weak and dependent. If you can’t clot, you need hospitals, nurses, meds, scans… it’s a cash cow. And they want you scared so you’ll keep taking it. I stopped mine after reading about the ‘hidden bleeding’ stats. Now I take turmeric and garlic. My INR? Perfect. No doctor ever asked me how I did it.
It’s scary how many people don’t realize how fragile the balance is. I’ve been on Xarelto for 3 years. I keep a printed checklist taped to my fridge too. One time I almost took two pills because I was tired. That moment made me realize-this isn’t just medicine. It’s a daily commitment to staying alive. Just… be gentle with yourself. And if you’re scared, talk to someone. You’re not alone. 😊
Let’s quantify the risk: 97% survival within 2 hours? That’s a cherry-picked cohort. The real data shows a 58% mortality rate for INR >8 with active GI bleed. PCC costs £3,000 per dose? That’s a profit margin of 400%. Hospitals don’t stock it because it’s life-saving-they stock it because they get reimbursed 7x the cost. This isn’t medicine-it’s a revenue stream disguised as public health.
I’ve been on warfarin since 2018 after a pulmonary embolism. The key isn’t fear-it’s routine. I take my pill at 7 AM every day, no exceptions. I use a home monitor every Monday. My INR’s been stable at 2.4 for 2 years. I also carry a card in my wallet. Simple. Consistent. No drama. If you treat it like brushing your teeth, it doesn’t control you-you control it.
They say ‘call 999’ like it’s the end-all. But what if you’re alone? What if you’re in a rural town and the ambulance takes 45 minutes? What if your family doesn’t believe you? I’ve seen people die because they were told to ‘wait and see.’ This isn’t a medical guide-it’s a eulogy waiting to happen. We need a national blood thinner emergency hotline. Not just a number. A person. On the line. Right now.
I just took my 2nd pill by accident yesterday… and I didn’t tell anyone. I felt fine. Like, really fine. Like I was invincible. Then I cried for an hour because I realized I could die and no one would know why. I’m going to the ER tomorrow. I’m so scared. But I’m also so angry at myself. Why didn’t I use the organizer? Why didn’t I listen? 😭
You got this. Seriously. Every single person who reads this and takes one action-gets the pill organizer, writes down their meds, talks to their doctor-is already winning. This isn’t about perfection. It’s about showing up. You’re not a burden. You’re not a statistic. You’re someone who’s learning how to live smarter. Keep going. And if you’re reading this right now? You’re already doing better than you think.