
Skeletal Muscle Condition Explorer
Treatment Plan Overview
Recommended Interventions:
Recovery Timeline:
Common Skeletal Muscle Conditions
Muscle Strain
Overstretch or partial tear of muscle fibers, graded I-III.
Muscle Tear
Complete break in the muscle, often requiring intensive rehab.
Myofascial Pain
Trigger points causing referred pain and restricted movement.
Chronic Pain
Persists beyond normal healing window, often due to posture or overuse.
Sports Injury
Common in active adults like hamstring pulls or calf strains.
Did you know that more than 30% of adults will face a muscle injury that limits daily activity at some point? When that happens, many assume rest and painkillers are enough, but the real game‑changer is physical therapy. By targeting the root causes, it can shave weeks-or even months-off recovery time.
When we talk about Physical therapy is a healthcare specialty that uses movement, manual techniques, and education to restore function, reduce pain, and prevent future injuries. It blends science and hands‑on care, making it ideal for tackling a wide range of muscle problems.
What counts as a skeletal muscle condition?
Broadly, any disorder that affects the contractile tissue of the musculoskeletal system falls under this umbrella. Here are the most common culprits:
- Muscle strain is an overstretch or partial tear of muscle fibers, often graded I‑III based on severity.
- Muscle tear (or rupture) involves a complete break in the muscle, typically requiring more intensive rehab.
- Myofascial pain syndrome is characterized by trigger points-tight knots in the fascia-that cause referred pain and restricted movement.
- Chronic musculoskeletal pain persists beyond the normal healing window, often linked to poor posture or overuse.
- Sports injuries such as hamstring pulls or calf strains, which are especially prevalent in active adults.
How physical therapy tackles each condition
Physical therapists (PTs) don’t use a one‑size‑fits‑all plan. Instead, they blend several evidence‑based approaches. Below are the core modalities that get the most mileage.
Exercise therapy
Exercise therapy involves progressive loading, stretching, and motor‑control drills designed to rebuild strength and flexibility. For a Grade II hamstring strain, a typical protocol starts with low‑intensity isometric holds, graduates to concentric/eccentric curls, and ends with sport‑specific agility drills.
Manual therapy
Manual therapy includes joint mobilizations, soft‑tissue massage, and trigger‑point release. In myofascial pain syndrome, therapist‑applied pressure on trigger points can instantly reduce referred pain and improve range of motion.
Neuromuscular re‑education
Neuromuscular re‑education focuses on retraining the brain‑muscle loop through balance, proprioception, and gait training exercises. After a calf rupture, patients often struggle with ankle stability; using wobble boards and single‑leg hops restores neural pathways faster than strength work alone.
Gait training
When an injury alters walking patterns, gait training corrects stride length, foot strike, and pelvic alignment. Clinics use treadmill biofeedback or over‑ground drills to prevent compensatory stresses that could spark new injuries.

Core PT interventions at a glance
| Technique | Primary Goal | Typical Conditions | Evidence Rating |
|---|---|---|---|
| Exercise therapy | Strength, flexibility, endurance | Strains, tears, chronic pain | High (systematic reviews) |
| Manual therapy | Reduce pain, improve tissue extensibility | Myofascial pain, mild sprains | Moderate‑high |
| Neuromuscular re‑education | Restore motor control, proprioception | Post‑rupture, balance deficits | High |
| Gait training | Normalize walking mechanics | Compensatory gait, post‑surgical | Moderate |
Why the results matter: data you can trust
Multiple studies published between 2018‑2024 show that early PT involvement cuts total downtime by 30‑45% compared with rest‑only protocols. A 2022 randomized trial on Grade III muscle tears reported an average return‑to‑sport time of 6weeks with PT versus 10weeks without.
Beyond speed, quality of recovery improves. Patients who completed a structured PT program reported 25% lower recurrence rates over a 12‑month follow‑up period.

Who should consider physical therapy?
If any of the following apply, PT is worth a look:
- Persistent pain >3days after a minor injury.
- Visible swelling or bruising that limits movement.
- Difficulty performing daily tasks-climbing stairs, lifting groceries, or reaching overhead.
- History of recurrent muscle injuries.
- Preparing for a high‑impact sport or returning after surgery.
Even asymptomatic individuals can benefit from preventive PT programs that enhance muscle balance and reduce future injury risk.
Tips to maximize your PT outcomes
- Ask for a clear goal sheet. Your therapist should write down short‑term (e.g., pain ↓ 50% in 2 weeks) and long‑term (return to running) targets.
- Do the home program. Consistency at night or on off‑days often determines success.
- Track pain and progress. Simple logs help therapists tweak intensity before a setback occurs.
- Stay hydrated and eat protein‑rich meals. Muscles repair faster with adequate nutrients.
- Communicate openly. If a movement feels “off,” let the PT know-adjustments are part of the process.
Frequently Asked Questions
How soon after an injury should I start physical therapy?
For most strains and tears, beginning PT within 48‑72hours-once acute swelling is under control-optimizes healing. Delaying beyond a week can lead to scar tissue that hampers flexibility.
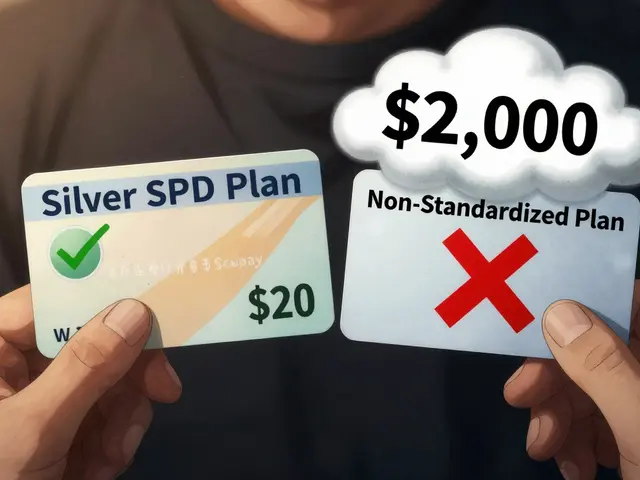
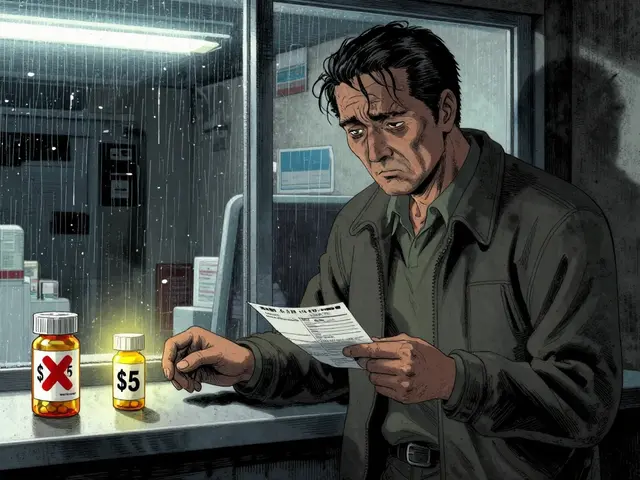
Will insurance cover the cost of PT?
Most major U.S. health plans cover PT when a physician orders it, usually with a copay. Check your policy for session limits and any pre‑authorization requirements.
Can I do PT exercises at home?
Absolutely. Therapists often provide printed or digital home‑exercise sheets. Consistent at‑home work usually halves recovery time compared with clinic‑only sessions.
What’s the difference between a muscle strain and a tear?
A strain is a partial tear of fibers (Grades I‑III). A full‑thickness tear or rupture means the muscle is split into two separate ends, often requiring more intensive rehab or even surgery.
Are there risks if I skip physical therapy?
Skipping PT can lead to chronic pain, weakness, and a higher chance of re‑injury. In some cases, unaddressed scar tissue can cause joint stiffness that may require surgical intervention later.




15 Comments
Physical therapy is a beacon-cutting weeks off recovery! Embrace movement, conquer pain!
Excellent overview! The emphasis on progressive loading really highlights how PT accelerates healing while maintaining safety.
The article correctly identifies exercise therapy as fundamental; however, it neglects to address the importance of periodized strength protocols, which are essential for preventing re‑injury. A more rigorous inclusion of periodization would elevate the clinical relevance.
Great summary, and it’s crucial to remember that cultural beliefs can influence patients’ adherence to home‑exercise programs.
While the data presented is compelling, one might consider the socioeconomic factors that affect access to PT services, especially in rural settings.
It is an ethical imperative that society allocates sufficient resources to physical therapy; neglecting this duty exacerbates chronic suffering and undermines our collective well‑being.
Love how the article breaks down each technique! 😊 Keep spreading the PT love!
Yo bro, PT actually kick's butt for those ripped muscles, no doubt!
PT reduces recovery time dramatically.
Wow-another article preaching the same old PT hype!!! Nothing new, just rehashed fluff!!!
Stop waiting for pain to vanish on its own-hit the gym with a PT plan now and dominate your rehab!
Only amateurs ignore the proven neuromuscular protocols; smart athletes follow them.
One cannot help but notice the article’s pretentious reverence for conventional PT paradigms. It extols the virtues of exercise therapy as if it were the sole arbiter of musculoskeletal salvation, while silently marginalizing emerging modalities. Such selective glorification betrays a scholarly myopia that would make even a seasoned guru wince. Moreover, the prose oscillates between lofty diatribes and pedestrian summaries, leaving the reader in a perpetual state of disorientation. In short, the piece is a dramatic tableau of well‑intentioned but myopic advocacy.
Your emphasis on patient education truly resonates; clear goals empower recovery. Let’s keep fostering that collaborative spirit.
Reading through this comprehensive guide reminded me of the countless hours I’ve spent watching patients transform under the guidance of skilled physical therapists.
First, the distinction between a strain and a complete tear cannot be overstated; the rehabilitation pathways differ dramatically, and understanding that nuance sets the stage for realistic expectations.
Second, the integration of manual therapy with targeted exercise protocols creates a synergistic effect, accelerating tissue remodeling while preserving joint integrity.
Third, neuromuscular re‑education, often overlooked, is essential for re‑establishing proprioception, especially after high‑impact injuries like calf ruptures.
Fourth, gait training is not merely a finishing touch; it corrects compensatory patterns that, if left unchecked, can lead to secondary injuries.
Fifth, the evidence cited from 2018‑2024 robustly supports early PT involvement, consistently showing a 30‑45% reduction in downtime.
Sixth, patient adherence to home exercises remains the single biggest predictor of successful outcomes; without it, even the best in‑clinic program will falter.
Seventh, nutrition and hydration, though sometimes brushed aside, play a crucial role in muscle repair, underscoring the need for a holistic approach.
Eighth, insurance coverage, while generally favorable, varies widely; patients must navigate pre‑authorizations to avoid unexpected costs.
Ninth, cultural considerations influence how patients perceive pain and therapy, making culturally sensitive communication vital.
Tenth, the table summarizing techniques serves as an excellent quick reference for clinicians designing individualized plans.
Eleventh, recurring pain beyond three days should trigger a timely PT referral to prevent chronicity.
Twelfth, the article’s FAQ section addresses common misconceptions, but could expand on the role of tele‑rehab in today’s digital age.
Thirteenth, the emphasis on goal‑setting aligns with modern motivational strategies, fostering patient ownership.
Fourteenth, ongoing research into biologics and regenerative therapies may soon complement PT, offering a multimodal arsenal for clinicians.
Fifteenth, ultimately, physical therapy is not just a service; it is a partnership that restores function, confidence, and quality of life.