Methadone QT Prolongation Risk Calculator
This calculator estimates your risk of methadone-induced QT prolongation based on key factors. It's important to remember this is a simplified tool for educational purposes only. Always consult with your healthcare provider for clinical decisions.
Enter your information above to see your estimated QT risk.
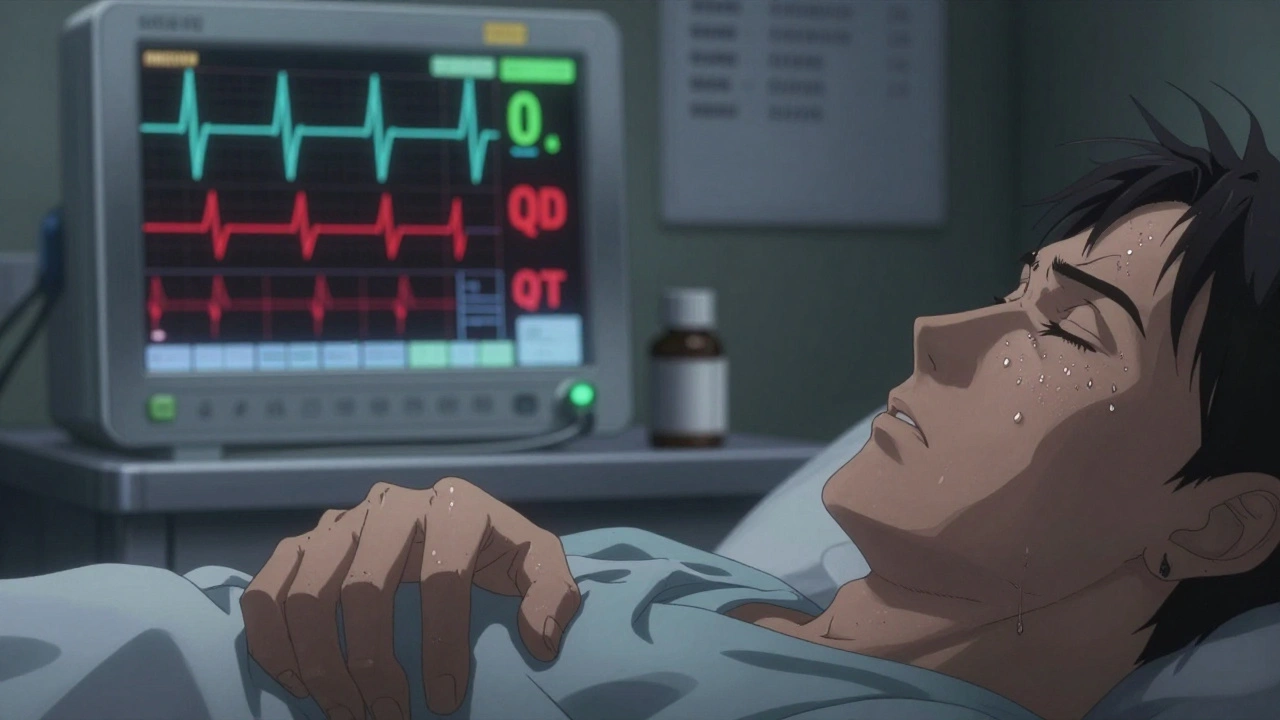
When you start methadone for opioid dependence, the goal is clear: stabilize your life, reduce cravings, and lower the risk of overdose. But behind that promise is a hidden danger many don’t talk about-methadone QT prolongation. It’s not a common side effect, but when it happens, it can be deadly. And unlike an overdose, there’s no obvious sign. No vomiting, no pinpoint pupils, no collapse. Just a quietly stretched-out heartbeat on an ECG that could lead to Torsades de Pointes-a dangerous arrhythmia that can kill without warning.
Why Methadone Stretches Your Heart’s Electrical Cycle
Methadone works by binding to opioid receptors in the brain, but it doesn’t stop there. It also blocks a specific potassium channel in heart cells called hERG (KCNH2). This channel is responsible for resetting the heart’s electrical charge after each beat. When it’s blocked, the heart takes longer to recharge. That delay shows up on an ECG as a longer QT interval-the time between the start of the Q wave and the end of the T wave. A normal QTc (corrected for heart rate) is under 430 ms for men and under 450 ms for women. Once it crosses 450 ms in men or 470 ms in women, you’re in the danger zone. At 500 ms or higher, your risk of sudden cardiac death jumps fourfold. This isn’t theoretical. Between 2000 and 2022, the FDA recorded 142 confirmed cases of Torsades de Pointes linked to methadone. Many more likely went unreported because sudden deaths in people on methadone are often labeled as overdose-even when the heart stopped first.Who’s at Highest Risk?
Not everyone on methadone develops QT prolongation. But certain factors stack the deck. If you’re a woman over 65, with low potassium, on other heart-affecting meds, or taking more than 100 mg a day, your risk isn’t just higher-it’s serious. Here’s what actually matters:- Dose: Risk rises with dose, but it’s not linear. Someone on 150 mg/day might have a QTc of 460 ms, while another on 200 mg might stay at 440 ms. Still, doses above 100 mg/day triple your risk.
- Gender: Women are 2.5 times more likely than men to develop dangerous QT prolongation. Why? Hormonal differences affect how methadone is metabolized and how heart cells respond.
- Electrolytes: Potassium below 3.5 mmol/L or magnesium below 1.5 mg/dL makes QT prolongation much more likely. Many people on methadone have poor nutrition or vomiting from other drug use-this isn’t rare.
- Other meds: Mixing methadone with antidepressants like amitriptyline, antipsychotics like haloperidol, or antibiotics like moxifloxacin can push QTc into the red zone. Even some common SSRIs like fluvoxamine can raise methadone levels by 50%.
- Heart disease: If you’ve had a heart attack, have heart failure (ejection fraction under 40%), or have a family history of sudden cardiac death, you’re at higher risk.
- Sleep apnea: About half of people on methadone have undiagnosed sleep apnea. Each time you stop breathing at night, your oxygen drops. That stresses the heart and makes arrhythmias more likely.
When and How to Monitor with ECG
You don’t need an ECG every week. But skipping it entirely is dangerous. Guidelines from SAMHSA and the American Heart Association agree: baseline ECG is non-negotiable. Here’s the real-world protocol:- Before starting: Get an ECG. Measure your QTc. If it’s already over 450 ms (men) or 470 ms (women), methadone may not be the right choice.
- At steady state: Wait 2-4 weeks after starting or changing your dose. That’s when methadone levels stabilize. Repeat the ECG.
- Monitor based on risk:
- Low risk: QTc under 450 ms (men) or 470 ms (women), no other risk factors → every 6 months.
- Moderate risk: QTc 450-480 ms (men), 470-500 ms (women), or 1-2 risk factors → every 3 months.
- High risk: QTc over 480 ms (men), 500 ms (women), or 3+ risk factors → monthly ECG, consider lowering dose or switching to buprenorphine.
- Red flags: If QTc increases by more than 60 ms from baseline, or hits 500 ms or higher, stop increasing the dose. Correct electrolytes. See a cardiologist. Consider switching.
What to Do If Your QTc Is Too High
If your ECG shows QTc over 480 ms, don’t panic. But don’t ignore it either. First, check your blood work. Potassium and magnesium are cheap, fast tests. If they’re low, correct them. Oral supplements often work, but sometimes IV is needed. Second, review every other medication you take. Are you on an antidepressant? An antifungal like fluconazole? An antibiotic? These can amplify methadone’s effect. Your prescriber may need to switch you to a safer alternative. Third, consider buprenorphine. It’s just as effective for opioid dependence but carries a fraction of the cardiac risk. Studies show buprenorphine rarely prolongs QTc, even at high doses. If you’re high-risk, it’s not just an alternative-it’s the smarter choice.Why Most Clinics Get This Wrong
Here’s the ugly truth: many methadone clinics don’t follow the guidelines. A Reddit survey of 142 patients in recovery found that 68% had inconsistent ECG monitoring. Some clinics did it once and never again. Others didn’t do it at all. But patients who got regular ECGs? 82% felt safer. Only 47% of those without monitoring did. That’s not just about data-it’s about trust. When you know your heart is being watched, you’re more likely to stick with treatment. A 2023 study in JAMA Internal Medicine showed that clinics with structured QT monitoring cut serious cardiac events by 67%. That’s not a small win. That’s life-saving.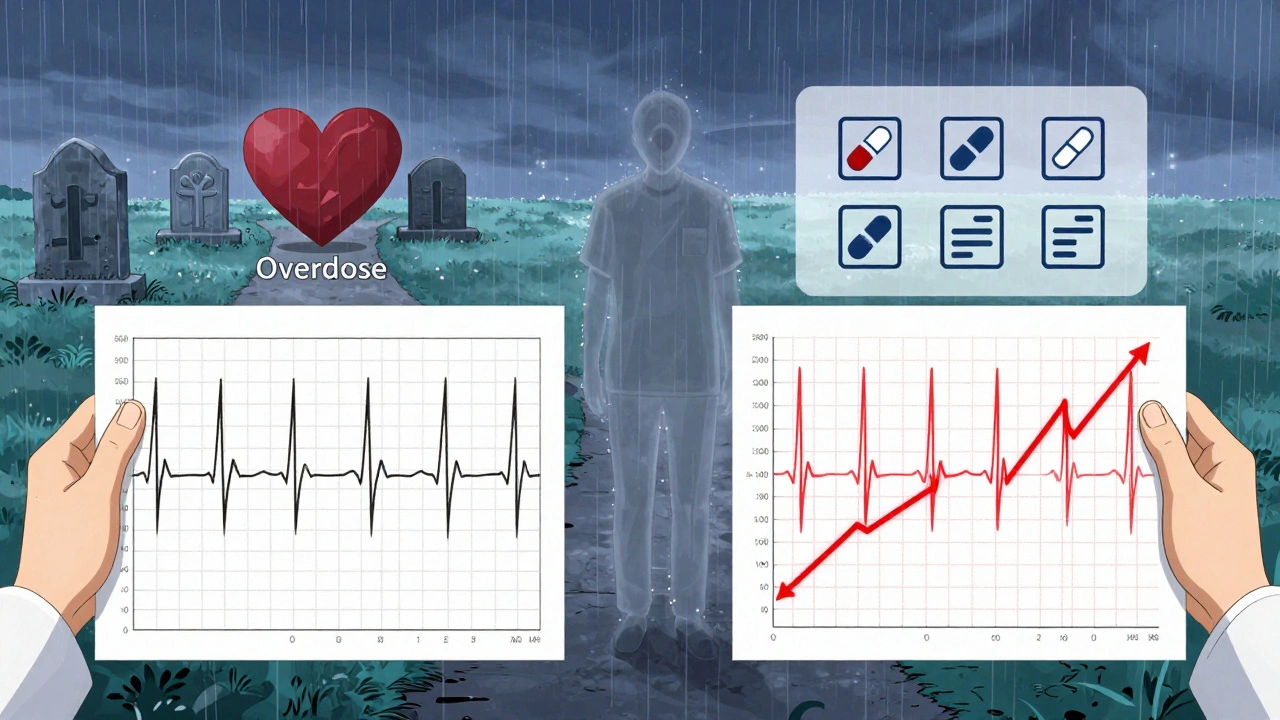
The Bigger Picture: Safety Doesn’t Mean Stopping Treatment
Methadone saves lives. People on methadone are 33% less likely to die than those not in treatment. It reduces crime, cuts HIV transmission, and gives people back their stability. That’s why we don’t stop prescribing it. We just make it safer. The answer isn’t fear. It’s vigilance. Baseline ECG. Regular checks. Correcting electrolytes. Avoiding dangerous drug combos. Knowing when to switch to buprenorphine. You’re not weak for needing monitoring. You’re smart for asking for it.What You Can Do Right Now
If you’re on methadone:- Ask your clinic: “When was my last ECG? When is the next one due?”
- Get your potassium and magnesium levels checked at least once a year.
- Make a list of every medication you take-prescription, over-the-counter, supplements-and review it with your prescriber.
- If you snore, gasp at night, or wake up exhausted, ask about sleep apnea testing.
- If your dose is over 100 mg/day and you have any risk factors, push for monthly ECGs.
- Don’t assume low-risk patients don’t need ECGs. Risk factors can appear suddenly.
- Keep a log of QTc values over time. A single reading isn’t enough.
- Have a plan for when QTc exceeds 500 ms. Don’t wait for a crisis.
- Know when to refer to cardiology. You don’t need to be the expert-you just need to know when to call one.






8 Comments
Methadone-induced QT prolongation is a well-documented hERG channel blockade phenomenon, and the clinical implications are non-trivial. The corrected QT interval (QTc) threshold of 450 ms for males and 470 ms for females is grounded in robust electrophysiological data. Beyond dose-dependent risk, concomitant use of CYP3A4/2B6 inhibitors-like fluvoxamine or certain antifungals-can elevate plasma methadone concentrations by up to 50%, compounding the arrhythmogenic potential. Electrolyte repletion, particularly potassium and magnesium, is not adjunctive-it’s foundational. Regular ECG monitoring at 2–4 weeks post-dose titration is standard of care per SAMHSA and AHA guidelines. Skipping it isn’t negligence; it’s malpractice.
Let’s be real-this whole ‘ECG monitoring’ thing is just another way for Big Pharma and the clinic system to keep you hooked. They don’t care if you live or die, they just want your monthly co-pay. I’ve seen people get kicked out of programs for having a QTc over 500, but nobody ever asks why their potassium’s low. Why? Because the clinics don’t feed you right. They serve you canned beans and saltine crackers while charging you $300 a month. And don’t get me started on how they push buprenorphine like it’s the holy grail-same drug, different name, same profit margin. They’re not protecting your heart. They’re protecting their bottom line.
It is, regrettably, the case that the dissemination of clinical guidelines regarding methadone-associated QT prolongation remains inconsistent across institutional settings. While the evidence base is robust, implementation is often haphazard, particularly in publicly funded outpatient clinics where resources are constrained. The absence of standardized protocols, coupled with inadequate staff training, results in significant variability in monitoring practices. This is not merely a clinical oversight; it is a systemic failure in the delivery of evidence-based care.
I appreciate the clarity here, especially the breakdown of risk factors. It’s easy to overlook how much nutrition and sleep apnea play into cardiac risk when you’re focused on addiction recovery. But you’re right-potassium and magnesium aren’t luxuries. They’re necessities. I’ve worked with folks who’ve been on methadone for years and never had a single lab check. That’s not care. That’s neglect wrapped in good intentions. If we’re serious about recovery being about living, not just surviving, then we need to treat the whole person. That means labs. That means ECGs. That means asking about snoring at 3 a.m. It’s not extra. It’s essential.
Oh please. You’re acting like this is some groundbreaking revelation. I’ve been in recovery for 12 years. Every clinic I’ve been to has done an ECG on day one. Some even did it monthly. The real problem isn’t the lack of monitoring-it’s the people who think they’re too ‘stable’ to need it. I had a friend die of Torsades at 68 mg. No high dose. No other meds. Just low magnesium and a genetic variant nobody tested for. This isn’t about rules-it’s about humility. You don’t get to decide you’re safe. The ECG does.
So let me get this straight-you want us to monitor QT intervals like we’re managing a cardiac ICU, but we’re still treating addicts like they’re disposable? You think telling someone to ‘get their potassium checked’ fixes the fact that they’re homeless, traumatized, and on a $100/month budget? This isn’t medicine. It’s performative compliance. You’re not saving lives-you’re checking boxes so your clinic doesn’t get audited. And don’t even get me started on buprenorphine. That’s just methadone with a prettier label and a higher price tag. The system doesn’t care if you live. It just cares if you look like you’re getting better.
Heart beats. Methadone slows the beat. Too slow, and it stops. Simple. You don’t need a 2000-word essay. You need a doctor who checks your heart before they give you the bottle. And if they won’t? Walk away. Your life’s worth more than their paperwork.
Oh wow, another sanctimonious post from someone who’s never been on methadone. You talk about ‘risk factors’ like you’re a cardiologist. Did you even have a QTc done? Or are you just reading guidelines on your iPhone while your kid’s in the next room screaming because you’re too high to parent? I’ve been on 150 mg for 7 years. My QTc is 442. I don’t take anything else. My potassium’s fine. I sleep like a log. So why am I the villain here? Because I didn’t cry about it on Reddit? You people are the reason addicts don’t trust doctors. You turn survival into a checklist. And then you act surprised when we stop showing up.