When you’re younger, a pill works the way it’s supposed to. You take your antibiotic, it clears the infection. You take your blood pressure pill, your numbers drop. But as you get older, especially past 65, that same pill might not work the same way - or worse, it might cause problems you never expected. This isn’t about being weak or frail. It’s about your body changing, and those changes affect how drugs are absorbed, processed, and how they affect you.
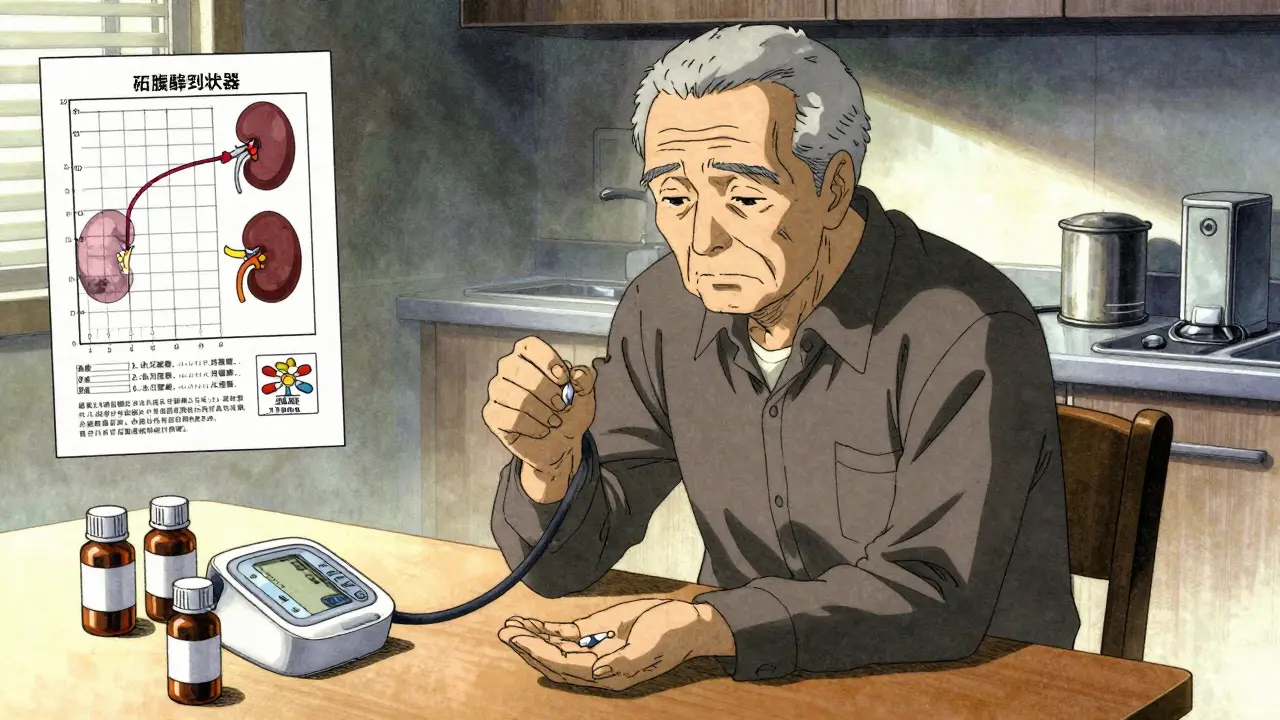
Your Kidneys Slow Down - and That Changes Everything
Your kidneys don’t just get weaker with age; they lose about 0.8 mL of filtering capacity per minute per 1.73m² of body surface area every year after 40. By the time you’re 80, you’re clearing drugs through your kidneys at 30-50% less efficiency than when you were 30. That means drugs like digoxin, aminoglycosides, or even common painkillers like ibuprofen stick around longer in your system. If your dose hasn’t been adjusted, you’re not just getting the right amount - you’re getting too much.
This is why doctors now check creatinine clearance instead of just looking at serum creatinine levels. A normal creatinine number doesn’t tell the full story in older adults because muscle mass declines with age, making creatinine misleading. The Cockcroft-Gault equation gives a more accurate picture of kidney function. If your creatinine clearance drops below 60 mL/min, about 40% of commonly prescribed medications need a lower dose - or to be switched entirely.
Your Liver Can’t Process Drugs Like It Used To
While your kidneys handle the cleanup, your liver does the heavy lifting: breaking down drugs so they can be eliminated. By age 70, liver blood flow drops by 30-40%. That means drugs that rely on liver flow - like propranolol, lidocaine, or even some antidepressants - get processed slower. The result? Higher drug levels in your blood for longer periods. You might feel drowsy, dizzy, or confused - not because you’re overdosing on purpose, but because your body can’t clear the drug fast enough.
Some drugs are metabolized by enzymes in the liver called CYP450. These enzymes become less active as you age. By 75, CYP2D6 activity - which handles about 25% of all medications - drops by 25%. That’s why some older adults react strongly to medications they’ve taken for years without issue. The drug isn’t new. Your body just changed.
Body Fat Goes Up, Water Goes Down - Drug Distribution Shifts
Between ages 25 and 75, body fat increases from about 25% to 35-40% in men and 35% to 45-50% in women. At the same time, total body water drops by 10-15%. This changes how drugs spread through your body.
Lipid-soluble drugs - like diazepam (Valium), amitriptyline, or even some sleep aids - dissolve into fat. With more fat, they get stored longer. That’s why a 5 mg dose of diazepam that worked fine at 50 might make you groggy and unsteady at 80. The drug isn’t stronger. It’s just sitting in your body longer.
On the flip side, water-soluble drugs - like lithium or certain antibiotics - don’t spread as widely because there’s less water to carry them. That can lead to higher concentrations in your blood, increasing the risk of toxicity even if the dose hasn’t changed.
Proteins Carry Drugs - But Older Bodies Carry Less
Many drugs, like warfarin, phenytoin, and some antibiotics, bind to proteins in your blood - mainly albumin - to stay inactive until they reach their target. As you age, your liver makes less albumin. Serum albumin drops from about 4.5 g/dL in young adults to 3.8 g/dL by age 80.
That means more of the drug floats around unbound - the active, dangerous kind. A standard dose of warfarin might be safe for a 50-year-old but could send an 80-year-old’s INR sky-high, leading to dangerous bleeding. That’s why older adults often need 20-30% lower doses of warfarin to stay in the therapeutic range.
Your Brain Gets More Sensitive - Even to Common Pills
It’s not just about how your body handles drugs. It’s about how your brain responds to them. Older brains have fewer neurons, a more permeable blood-brain barrier, and reduced receptor function. That makes you more sensitive to drugs that affect the central nervous system.
Benzodiazepines - like lorazepam or alprazolam - are a classic example. At 25, you might take 0.5 mg for anxiety and feel calm. At 75, that same dose can cause confusion, falls, or even delirium. Studies show older adults are 2-3 times more sensitive to these drugs. The American Geriatrics Society Beers Criteria lists them as potentially inappropriate for seniors because the risks outweigh the benefits.
Even over-the-counter meds like diphenhydramine (Benadryl) can cause serious problems. In people over 75, anticholinergic drugs like this cause confusion in 25% of users, urinary retention in 15-20%, and dizziness in 30%. Compare that to just 5-8% confusion and 3-5% urinary issues in people under 60. That’s not coincidence - it’s biology.
Why Your Heart Doesn’t Respond the Same Way
Your heart changes too. Beta-adrenergic receptors - which respond to adrenaline and medications like beta-blockers - decline by 40-50% in function between ages 20 and 70. That means drugs like propranolol or metoprolol don’t slow your heart as effectively. But here’s the twist: your blood vessels still respond to alpha-receptors. So while your heart doesn’t react as strongly, your blood pressure can still spike from stress or certain medications.
This is why some older adults on beta-blockers still have high blood pressure - not because the drug isn’t working, but because their receptors are worn out. Sometimes, switching to a different class of medication - like a calcium channel blocker - makes more sense than increasing the dose.
What You Can Do - Practical Steps for Safer Medication Use
Knowing these changes isn’t enough. You need to act on them.
- Start low, go slow. Doctors should begin with 25-50% of the standard adult dose for seniors, especially for drugs cleared by the kidneys. Many pharmacists now follow this rule for patients over 75 - and 82% report better outcomes.
- Ask about anticholinergic burden. If you’re taking multiple meds - even antihistamines, bladder pills, or antidepressants - ask your doctor to run your list through the Anticholinergic Cognitive Burden Scale. A score above 3 increases dementia risk by 50% over seven years.
- Use the Beers Criteria. It’s not just a list - it’s a tool. The American Geriatrics Society’s Beers Criteria updates annually and flags 30+ drug classes that should be avoided or adjusted in older adults. Many hospitals use it. Your pharmacist can too.
- Review meds every 6 months. Don’t wait for a crisis. Ask for a full medication review with your doctor or pharmacist. Many seniors take 5+ pills daily - and some are no longer needed. A 2021 study showed that regular reviews cut inappropriate prescribing by 35%.
- Track side effects. If you feel foggy, dizzy, constipated, or more forgetful after starting a new drug - don’t assume it’s just aging. It might be the pill.
What’s Changing in the Future
The FDA now requires all new drugs to include testing in adults over 65. Since 2018, 73% of approved medications include geriatric dosing guidance. In 2023, the first age-adjusted dosing algorithm for dabigatran (Pradaxa) was approved - reducing bleeding in patients over 80 by 31%.
Researchers are also exploring senolytics - drugs that clear out aging, damaged cells. Early trials show these can reduce inflammation and even restore some drug response in older tissues. It’s still experimental, but it points to a future where medications aren’t just adjusted for age - they’re designed for it.
Meanwhile, tools like DosemeRx and the Beers Criteria app are helping pharmacists and doctors personalize doses based on kidney function, weight, and other factors. These aren’t sci-fi - they’re in use in over 300 U.S. hospitals today.
Final Thought: Age Isn’t the Problem - Ignorance Is
Older adults aren’t more likely to have bad reactions to drugs because they’re old. They’re at higher risk because the system still treats them like younger people. A 78-year-old with kidney disease shouldn’t get the same dose of a drug as a 45-year-old with healthy kidneys. Yet it happens - often.
The solution isn’t more pills. It’s smarter prescribing. It’s asking: How does this drug work in a body that’s changed? It’s listening when patients say, “I feel different since I started this.” And it’s remembering that what worked at 50 might be dangerous at 80.
Medication isn’t one-size-fits-all. Especially not when you’re aging.
Why do older adults need lower doses of some medications?
Older adults often need lower doses because their bodies process drugs differently. Kidneys filter less efficiently, the liver breaks down drugs slower, body fat increases while water decreases, and protein levels drop - all of which cause drugs to stay in the system longer or become more active. Even the brain becomes more sensitive to certain medications, making standard adult doses too strong.
What medications should seniors avoid?
The American Geriatrics Society Beers Criteria lists 30+ medications to avoid or use with caution in older adults. These include benzodiazepines (like Valium), anticholinergics (like Benadryl), nonsteroidal anti-inflammatories (like ibuprofen), and certain antipsychotics. These drugs carry high risks of confusion, falls, kidney damage, or bleeding in seniors - and often have safer alternatives.
How can I tell if a medication is causing side effects?
Watch for new symptoms that started after beginning a new drug: confusion, dizziness, constipation, urinary problems, unsteady walking, or sudden fatigue. These aren’t normal aging - they’re red flags. Keep a journal of when symptoms occur and share it with your doctor. Many adverse reactions are reversible if caught early.
Is it safe to take over-the-counter meds as I age?
Not always. Common OTC drugs like diphenhydramine (in sleep aids and allergy meds), ibuprofen, and even some cold remedies have strong anticholinergic or kidney-stressing effects. Many seniors don’t realize these are drugs - and they can be just as risky as prescriptions. Always check with a pharmacist before taking any OTC product.
What’s the best way to manage multiple medications?
Get a full medication review at least once a year - or every six months if you’re on five or more drugs. Bring all your pills (or a list) to your doctor or pharmacist. Ask: Is this still needed? Could this interact with another? Is the dose right for my age and kidney function? Tools like the Beers Criteria app or Anticholinergic Burden Calculator can help guide these conversations.
For more information, consult your pharmacist or geriatric care provider. Never stop or change a medication without talking to your doctor - but do ask questions. Your body is different now. Your meds should be too.






13 Comments