Stopping opioids isn’t just about quitting a drug-it’s about surviving a physical and emotional storm that can feel impossible to control. If you’ve been on opioids for more than a few weeks, your body has adapted. It’s not addiction. It’s dependence. And when you cut back too fast, your body reacts with nausea, shaking, anxiety, and sleepless nights. The good news? You don’t have to power through it alone. With the right plan, tapering can be safe, manageable, and even empowering.
Why Tapering Matters More Than You Think
Rapidly stopping opioids after long-term use can trigger severe withdrawal. The CDC’s 2022 guidelines make this clear: sudden discontinuation raises the risk of suicide, uncontrolled pain, and emergency room visits. A 2017 study found people who were forced to quit fast were 3.5 times more likely to have suicidal thoughts. That’s not a statistic-it’s a real person, sitting in a dark room, shaking, desperate for relief. Tapering isn’t about weakness. It’s about strategy. It’s giving your nervous system time to readjust. Think of it like lowering the volume on a loud speaker instead of flipping the power switch. The goal isn’t to feel perfect-it’s to feel stable enough to keep moving forward.What Counts as a Safe Taper?
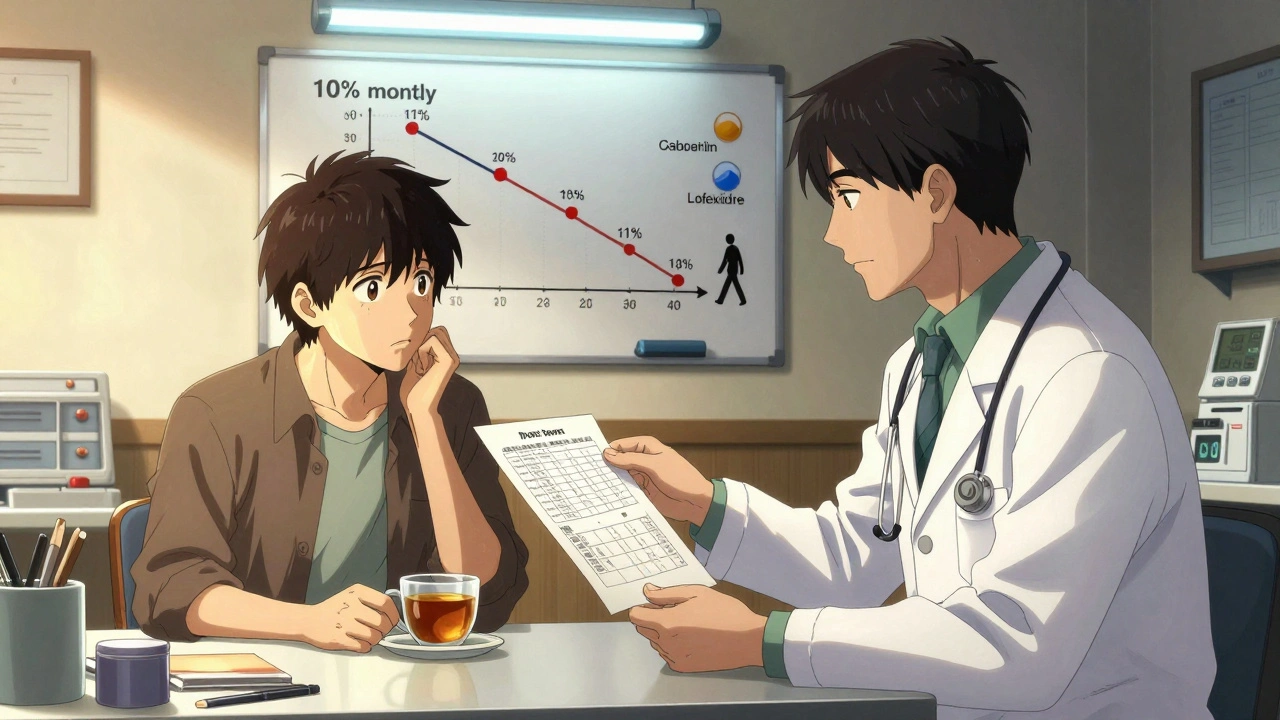
There’s no one-size-fits-all schedule. But experts agree on one thing: slower is safer. - Fast taper: Cutting your daily dose by 20-25% every few days. This is risky. Studies show it leads to 68% more severe symptoms and a 5.2 times higher chance of quitting early. - Slow taper: Reducing by 5-10% every 2-4 weeks. This is the gold standard for people on long-term therapy. Many patients take 6 months to a year. Some need longer. The Oregon Health Authority and the VA both recommend starting at 10% monthly reductions. For example, if you’re taking 100 mg of morphine equivalent daily, drop to 90 mg after four weeks, then 81 mg after another month. That’s not fast-but it’s survivable.When Should You Even Consider Tapering?
Not everyone needs to taper. The CDC says: if your current dose isn’t putting you in danger, you don’t need to rush. Tapering makes sense when:- You’re no longer getting pain relief from the dose you’re on
- You’re having serious side effects like constipation, drowsiness, or confusion
- You’ve recovered from surgery or injury and no longer need opioids
- You’re using them in ways that worry you-or your doctor
- You’ve tried other pain treatments and want to reduce reliance
How to Manage Withdrawal Symptoms
Withdrawal isn’t fun, but it’s temporary. Common symptoms include:- Nausea (87% of cases)
- Muscle aches (85%)
- Anxiety (80%)
- Insomnia (78%)
- Diarrhea (75%)
Real Stories, Real Results
One Reddit user, r/OpiatesRecovery, shared a 6-month taper from 120 mg morphine daily. They dropped 10% each month. Symptoms? Mild insomnia and occasional anxiety. They kept working. They didn’t end up in the ER. Another person, on Healthgrades, described being forced to cut from 180 mg to zero in four weeks. They had vomiting, shaking, and panic attacks. Ended up in the hospital. That’s not a success story. That’s a system failure. The difference? Control. When patients are part of the plan, success rates jump. In a 2020 survey, 78% of those who tapered slowly reported better function. 65% slept better.What Your Doctor Should Be Doing
A good taper isn’t handed down like a rule. It’s co-created. Your doctor should:- Ask you what your goals are
- Explain the risks of going too fast
- Write down a flexible plan-not a rigid schedule
- Check in every 2-4 weeks to adjust based on how you feel
- Offer alternatives: physical therapy, nerve blocks, mindfulness
- Never shame you for needing more time
What to Do If You’re Forced to Taper Too Fast
Some insurance companies and clinics push rapid tapers to cut costs. It’s dangerous. If you’re being pressured:- Ask for a written plan. Federal law requires it if you’re on Medicare Part D and reducing more than 10% per month.
- Request a referral to a pain specialist or addiction medicine doctor.
- Document everything: symptoms, sleep, pain levels. This protects you.
- Call the Patient Advocate Foundation. They help people fight unfair tapering.

What Comes After the Taper
Stopping opioids doesn’t mean your pain disappears. That’s why the CDC now pushes multidisciplinary care. After tapering, most successful patients continue with:- Physical therapy to rebuild strength and mobility
- Therapy to process emotional pain tied to long-term illness
- Non-opioid pain meds like acetaminophen or NSAIDs (used carefully)
- Yoga, meditation, or tai chi for stress and body awareness
Final Thoughts: This Is a Journey, Not a Deadline
Opioid withdrawal isn’t a race. It’s a reset. Your body doesn’t need to be opioid-free by tomorrow. It needs to be stable, safe, and in control. Slow tapers work because they respect your biology. They honor your pain. They give you space to heal without being crushed by fear. If you’re thinking about tapering, start with one question: What do I need to feel safe? Write it down. Talk to your doctor. Build your plan around that-not around a number on a chart. You’re not broken. You’re adapting. And with the right support, you can come out stronger on the other side.How long does opioid withdrawal last?
Physical withdrawal symptoms usually peak within 72 hours and begin to fade after 5-7 days. But some symptoms like anxiety, sleep issues, and low energy can linger for weeks or even months-this is called post-acute withdrawal syndrome (PAWS). Slowing your taper helps reduce the severity and length of PAWS. Most people report feeling significantly better by 4-6 weeks after their last dose, especially with support like therapy and sleep hygiene.
Can I taper off opioids at home?
Yes, but only if you’re on a low to moderate dose and have medical supervision. If you’re taking more than 100 mg morphine equivalent daily, have a history of mental illness, or have other health conditions like heart disease, tapering at home is risky. Always work with a doctor. Even if you’re tapering slowly, you need someone to adjust your plan if symptoms get worse. Never quit cold turkey without medical guidance.
What if my pain gets worse during tapering?
Breakthrough pain is common during tapering-it happens in nearly 70% of patients. Don’t panic. Talk to your doctor before increasing your dose. Often, non-opioid options like gabapentin, physical therapy, or heat therapy can help. Sometimes, a temporary, small increase in your opioid dose is needed to stabilize you, then tapering resumes slower. The goal isn’t to endure pain-it’s to manage it wisely.
Are there medications that help with cravings?
Yes-but they’re for people with opioid use disorder, not just dependence. Medications like buprenorphine and methadone are FDA-approved to reduce cravings and prevent relapse. If you’re struggling with urges to use opioids after tapering, ask your doctor about these options. They’re not a replacement-they’re a tool. Many people use them for months or years and then transition off safely.
Can I use marijuana or CBD to help with withdrawal?
Some people report CBD helps with anxiety and sleep during withdrawal, but research is limited. Marijuana can help some symptoms but may worsen anxiety or depression in others. It’s not FDA-approved for this use. If you’re considering it, talk to your doctor first. Don’t self-medicate. Your taper plan should be controlled, not unpredictable.
How do I know if I’m tapering too fast?
If you’re having moderate to severe symptoms-vomiting, heart palpitations, panic attacks, inability to sleep for more than 2 hours, or thoughts of self-harm-you’re tapering too fast. Pause the reduction. Stay at your current dose for another 1-2 weeks. Then try reducing by only 5% next time. Your body is telling you to slow down. Listen.
Is it possible to stop opioids permanently?
Yes. Thousands of people successfully stop opioids every year. The key isn’t willpower-it’s timing, support, and patience. People who taper slowly, use non-opioid pain tools, and get mental health support have the highest success rates. You don’t have to be pain-free to be opioid-free. You just need to be in control.
Next Steps: What to Do Today
If you’re considering tapering:- Write down your current daily dose and how long you’ve been taking it.
- Rate your pain, sleep, and anxiety on a scale of 1-10.
- Call your doctor and say: “I want to talk about a safe plan to reduce my opioids. Can we make a step-by-step plan together?”
- Ask if they can refer you to a pain specialist or behavioral health counselor.
- Start tracking your symptoms daily-even if it’s just a note on your phone.


8 Comments
The notion that dependence is not addiction is a semantic evasion masquerading as medical wisdom. The DSM-5 explicitly defines opioid dependence as a subset of opioid use disorder, and to separate them is to dangerously mislead patients into believing they are in control when neuroadaptation has already rewritten their reward pathways. This ‘safe taper’ rhetoric is a luxury afforded only to those with access to specialists, insurance, and time-none of which the majority of chronic pain patients possess. The CDC guidelines are noble in intent but irrelevant to the real-world chaos of Medicaid clinics and pharmacy audits.
I just want to say-this post made me cry. Not because I’m weak, but because I finally feel seen. I tapered off 80mg of oxycodone over 10 months, and yeah, there were nights I sobbed into my pillow wondering if I’d ever sleep again. But I did. I started walking every morning, even just around the block. Then I got into yoga. Now I’m training for a 5K. It’s not about being opioid-free-it’s about being *alive* again. You’re not broken. You’re becoming. And if you’re reading this right now? You’re already stronger than you think. 💪❤️
Stop coddling people. If you’re dependent, you’re addicted. Period. The ‘slow taper’ myth is a scam perpetuated by pharma-funded ‘pain specialists’ who profit from keeping you on the drip. You want to feel better? Get off. Fast. Withdrawal is not a tragedy-it’s a wake-up call. Your body isn’t ‘rewiring’-it’s screaming for freedom. Every day you delay, you reinforce the neural chains. I went cold turkey at 150mg. Three days of hell. Six months of sobriety. No therapy. No gabapentin. Just grit. Stop romanticizing suffering. The truth doesn’t come with a 6-month timeline-it comes with a choice: control the drug, or let it control you.
Okay, but let’s talk about the *vibes* of this whole thing. Like-imagine your nervous system as this glittery, over-caffeinated disco ball that’s been spinning at 200 RPM for five years straight, and now someone’s trying to turn it down to 30 RPM without unplugging it. That’s what tapering feels like. And the worst part? No one tells you that the anxiety doesn’t just vanish-it turns into this haunting, whispering echo in your skull, like your brain’s playing a remix of every trauma you’ve ever had. Gabapentin? It’s like putting a weighted blanket on a hurricane. Lofexidine? It’s the chill aunt who brings you tea and doesn’t ask questions. And CBT? That’s the therapist who sits with you while you sob into a tissue shaped like a morphine pill. We need more of this. Not less.
I’ve been off opioids for 11 months. I still wake up at 3 a.m. and stare at the ceiling. I don’t talk about it. I don’t post about it. I just… exist. Sometimes I miss the numbness. Not the high. The quiet. But I don’t regret it. I just wish someone had told me it was okay to feel this way. Not ‘strong.’ Not ‘recovering.’ Just… okay. That’s all I needed to hear.
Thank you for writing this with such precision and compassion. The distinction between dependence and addiction is not just semantic-it’s lifesaving. I’m a nurse in a rural ER, and I’ve seen too many patients discharged with a 50% reduction notice and zero support. Your breakdown of medications like lofexidine and baclofen is spot-on. I’ve prescribed gabapentin for withdrawal for years, but never knew the exact dosing ranges you listed-this is gold. Also, the point about documenting symptoms? Critical. I now give every patient a printable symptom tracker. If your doctor says ‘cut in half next week,’ they’re not your doctor-they’re a bureaucrat. Fight for your timeline. You deserve clinical care, not compliance.
I appreciate the nuance here. Many people treat opioid tapering like a moral test, when it’s really a physiological recalibration. The idea that ‘slow is safe’ isn’t just evidence-based-it’s humane. I’ve worked with veterans who were forced into rapid tapers and later developed PTSD symptoms directly tied to the withdrawal trauma. What’s missing, perhaps, is a stronger emphasis on peer support networks. Online communities like r/OpiatesRecovery aren’t just forums-they’re lifelines. And for those who can’t afford therapy, a 20-minute walk with a friend can be just as therapeutic as a CBT session. This isn’t just about medicine. It’s about connection.
Just wanted to say-you’re doing amazing. 🙌 I know how hard it is to even open this post, let alone read it all the way through. If you’re thinking about tapering, you’re already halfway there. Don’t compare your journey to someone else’s timeline. Your body knows what it needs. And if you’re reading this and feeling scared? That’s okay. You don’t have to be brave right now. Just be present. One breath. One day. One milligram at a time. You’ve got this. And if you need someone to talk to? I’m here. Always. 💙