Pre-Medication Protocol Calculator
Medical Procedure Type
Patient Information
Contrast-Specific Options
Chemotherapy Options
Steroid Protocol
Antihistamine Protocol
Antiemetic Protocol
Critical Timing Reminder
Why Pre-Medication Matters in Modern Medicine
Every year, millions of patients receive contrast dye for CT scans, MRIs, or angiograms. Others undergo chemotherapy for cancer. These procedures save lives-but they also carry risks. Some people react badly. Their skin breaks out in hives. Their blood pressure drops. They throw up uncontrollably. These aren’t rare accidents. They’re predictable, preventable events. That’s where pre-medication comes in.
Using antiemetics, antihistamines, and steroids before a procedure isn’t about being extra cautious. It’s about stopping reactions before they start. Hospitals and clinics don’t just guess at what works. They follow strict, research-backed protocols built over decades. The goal? Reduce severe reactions by more than 90%. That’s not a small win. It’s life-changing for patients who’ve had bad experiences before.
How These Three Drugs Work Together
These aren’t random pills thrown together. Each drug has a specific job.
- Steroids (like prednisone or methylprednisolone) calm the immune system. They stop the body from overreacting to contrast dye or chemo drugs. They take hours to work, so timing matters.
- Antihistamines (like cetirizine or diphenhydramine) block histamine, the chemical that causes itching, swelling, and redness. They act fast and help with mild reactions.
- Antiemetics (like ondansetron or aprepitant) stop nausea and vomiting before it begins. They’re especially critical for chemo patients, where vomiting can be worse than the cancer itself.
Together, they form a layered defense. Steroids handle the big-picture immune response. Antihistamines catch the early signs. Antiemetics protect the stomach. This isn’t just theory. Studies show this combo cuts moderate-to-severe reactions from 0.7% down to 0.04% in contrast imaging.
When and How to Use Them: The Real-World Rules
There’s no one-size-fits-all schedule. It depends on the patient, the procedure, and how fast you need results.
For outpatients with a past reaction to contrast dye, Yale’s protocol is widely used: 50mg prednisone taken orally at 13 hours, 7 hours, and 1 hour before the scan. Plus, 10mg cetirizine within an hour of the procedure. That 13-hour window is non-negotiable. Steroids need time to build up in the bloodstream.
For emergency or hospitalized patients, there’s no time for oral meds. Instead, they get 40mg methylprednisolone IV four hours before the scan. If that’s not available, 200mg hydrocortisone IV is the backup. Antihistamines here are given IV too: either 50mg diphenhydramine or 10mg cetirizine by mouth.
For kids, it’s all about weight. A child over 6 months gets cetirizine based on their size. Babies under 6 months get diphenhydramine at 1mg per kg-no more than 50mg total. Pediatric doses aren’t just scaled-down adult doses. They’re calculated precisely.

Antihistamines: First-Gen vs. Second-Gen
Not all antihistamines are created equal. The old standby, diphenhydramine (Benadryl®), works-but it knocks people out. One study found 42.7% of adults felt drowsy after taking it. That’s a problem if someone needs to drive home or care for kids after a scan.
Cetirizine (Zyrtec®), a second-generation antihistamine, is just as effective at preventing reactions-but only 15.3% of patients report drowsiness. That’s why most hospitals now prefer it. It’s safer, cleaner, and doesn’t interfere with daily life. The only catch? It costs more. But when you factor in lost work time and fall risks from dizziness, the price difference is worth it.
Antiemetics for Chemotherapy: The Triple Threat
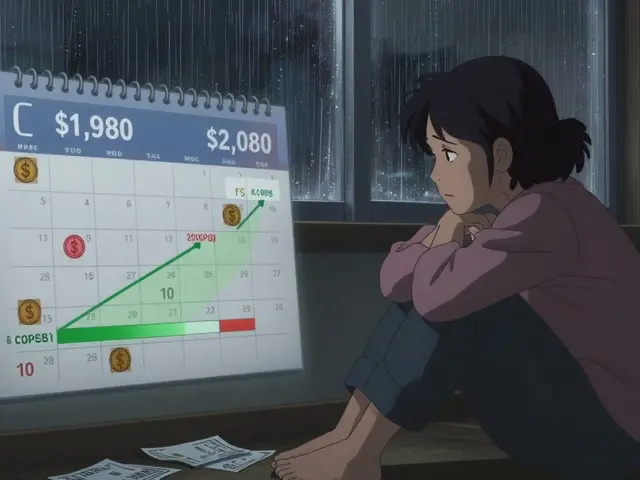
Chemo-induced nausea used to be accepted as normal. Not anymore. Today’s gold standard is a three-drug combo: a 5-HT3 antagonist (like ondansetron), an NK1 antagonist (like aprepitant), and dexamethasone (a steroid).
This triple therapy works in 70-80% of cases. That means most patients stay nausea-free for the first 24 hours after chemo. Compare that to old-school single-drug plans, which only worked about 50% of the time. A 2023 meta-analysis showed the triple combo reduced vomiting to 28.4%, while dual therapy left 56.7% of patients still sick.
But even this isn’t perfect. High-risk chemo drugs like cisplatin still cause breakthrough nausea in 15-20% of patients. That’s why nurses now track symptoms daily and adjust meds as needed. It’s not just about giving pills-it’s about listening to what the patient says.
The Hidden Risks: When Pre-Medication Goes Wrong
Even the best protocols can fail if they’re not followed correctly. Medication errors happen. A 2022 survey found that 68.3% of hospitals had mistakes in premedication orders. In 22.7% of those cases, the wrong dose reached the patient.
One common error? Mixing up oral and IV steroids. Giving IV methylprednisolone when the patient was supposed to take oral prednisone can lead to dangerous spikes in blood sugar or mood swings. Another? Forgetting to time the doses. If a patient takes their steroid at 8 AM but the scan is at 10 AM, they didn’t get the full benefit.
And here’s something many don’t realize: premedication doesn’t make you immune. About 4.2% of premedicated patients still get mild reactions. 0.8% still have moderate ones. That’s why staff always keep emergency meds and equipment ready-even if the patient took everything on time.
How Hospitals Are Fixing the Problems
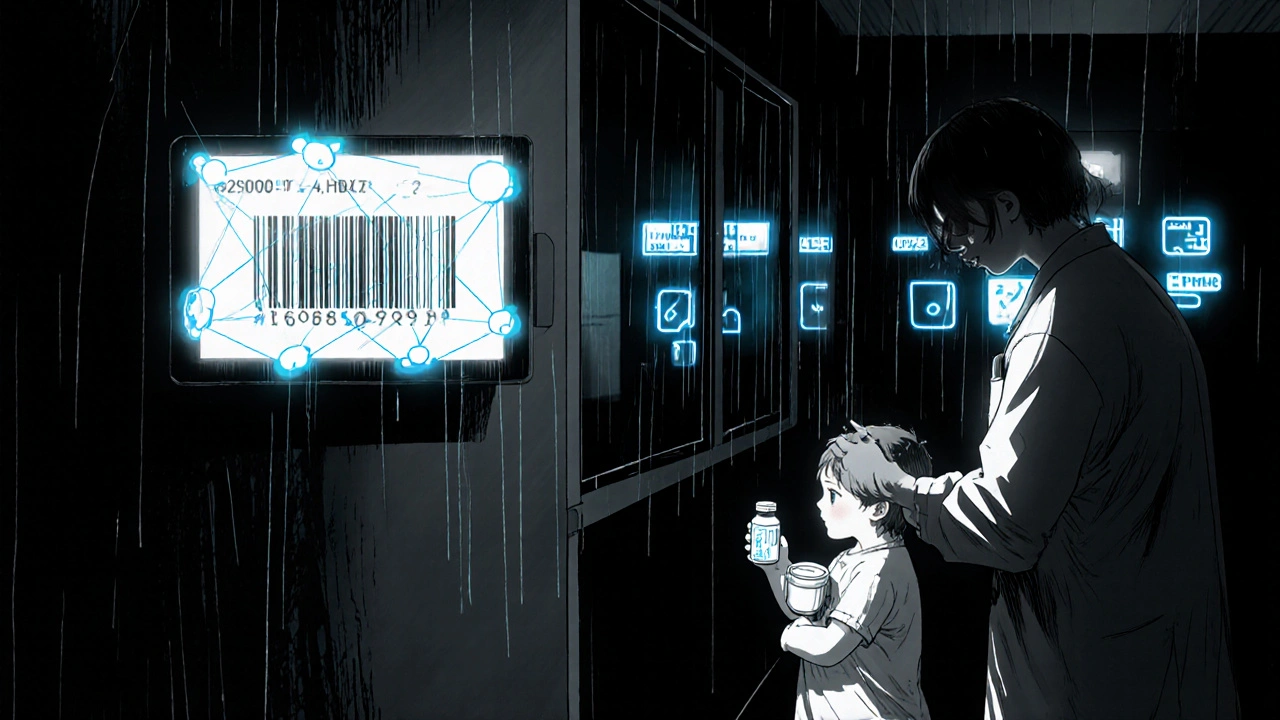
Smart hospitals aren’t just relying on staff memory. They’re building systems.
- Electronic health records now have automated alerts that pop up when a patient has a history of contrast reaction.
- Order sets are pre-built so doctors can’t accidentally skip a step.
- Barcode scanning ensures the right drug, right dose, right patient, right time.
Yale Medicine spent six months training radiology, pharmacy, and nursing teams before rolling out their protocol. After a year, 94.7% of staff followed it correctly. At Johns Hopkins, using barcode scans cut contrast reactions by 92%.
The Institute for Safe Medication Practices (ISMP) says the key is three phases: pre-intervention (training and reporting), intervention (using tools like checklists), and post-intervention (tracking outcomes). Facilities that do all three cut medication errors by nearly 38%.
What’s Next? AI and New Drugs
Science isn’t standing still. Researchers are now using machine learning to predict who’s most likely to react. A 2023 study trained an algorithm on over 10,000 patient records. It predicted contrast reactions with 83.7% accuracy-better than most human doctors.
On the drug front, new NK1 antagonists like fosnetupitant are coming. They’re longer-lasting, easier to give (single IV dose), and may replace older pills like aprepitant. The American Society of Clinical Oncology says these will likely become standard in the next 3-5 years.
But the big picture hasn’t changed: pre-medication isn’t going away. It’s getting smarter. The focus is no longer on giving everyone the same meds. It’s on giving the right meds to the right people at the right time.
What Patients Should Know
If you’re scheduled for a scan or chemo and told you need premedication, ask these questions:
- Why am I getting this? Did I have a reaction before?
- What time do I need to take each pill? What if I forget?
- Will I feel sleepy? Can I drive after?
- What if I still feel sick or itchy after?
Don’t assume it’s routine. Ask for the exact names and doses. Write them down. Tell your pharmacist. If you’re told you need steroids 13 hours before, plan your day around it. Skip your morning coffee if you’re taking oral meds-some interactions can reduce effectiveness.
And if you’ve never had a reaction before? You probably don’t need premedication. Studies show giving it to everyone doesn’t help-and it exposes you to unnecessary side effects. It’s only for those with a documented history.






11 Comments
Also, the drowsiness thing? I took Zyrtec and felt fine. My coworker took Benadryl and slept for 8 hours straight. No contest.
It's not about the drugs. It's about the system. We're engineering solutions for a world that doesn't exist anymore.
And don’t get me started on 'AI predicting reactions.' If you can predict it, why not just avoid the damn dye? Or use ultrasound? Or MRI without contrast? They don't want you to know the alternatives. They want you dependent.
And still, we call this medicine.