
When you pick up a generic pill, you expect it to work just like the brand-name version. You don’t expect it to be fake. But counterfeit drugs are real - and they’re more common than most people realize. In some countries, up to 30% of medicines sold online are fake. Even in places with strong regulations, like the U.S. and EU, counterfeiters are getting smarter. They copy packaging, label bottles correctly, and even get the chemical formula right. So how do we stop them? The answer isn’t just more inspections. It’s quality control built into every step of manufacturing.
Why Quality Can’t Be Tested In
Many assume that if a drug passes lab tests, it’s safe. That’s a dangerous myth. The U.S. Food and Drug Administration (FDA) made this clear decades ago: "Quality cannot be tested into a finished product; it must be built into the design and manufacturing process at every single step." Testing the final pill tells you if it contains the right ingredient. But it won’t tell you if the crystal structure is wrong, if the binder is toxic, or if the tablet disintegrates too slowly in your stomach. Those are the hidden flaws that make a drug useless - or dangerous. Take the 2018 valsartan recall. Hundreds of thousands of pills were pulled because a harmful impurity slipped through standard testing. The chemical was there. The dosage was correct. But the manufacturing process created a side reaction that wasn’t caught. That’s why quality control today isn’t about spot checks. It’s about controlling how the drug is made - from the raw powder to the sealed blister pack.The SQUIPP Framework: What Really Matters
Generic drug makers don’t just follow vague guidelines. They use a strict framework called SQUIPP: Safety, Quality, Utility (identity), Potency, and Purity. Each letter stands for a non-negotiable requirement.- Identity: Is this really the drug it claims to be? Infrared spectroscopy and high-performance liquid chromatography (HPLC) are used to match the molecular fingerprint of each batch to a reference standard. These tests can spot fake ingredients with 99.9% accuracy.
- Potency: Does it contain the right amount of active ingredient? Too little, and it doesn’t work. Too much, and it could overdose you. Batch samples must release 80% of the drug within 30 to 45 minutes in dissolution tests.
- Purity: Are there toxic contaminants? This includes heavy metals, solvents, or unintended chemical byproducts. Each batch is tested against strict limits set by pharmacopeias like USP or EP.
- Safety: Is the manufacturing environment clean? Clean rooms must meet ISO Class 5 standards - meaning no more than 3,520 particles per cubic meter larger than 0.5 microns. That’s like having fewer than 35 dust specks in a room the size of a small office.
- Quality: Is every step repeatable? Statistical process control tracks over 20 parameters per manufacturing step. If one value drifts, the whole batch is held.
How Digital Systems Block Counterfeits
Physical testing alone isn’t enough. Counterfeiters now use real active ingredients. So the next line of defense is digital. The U.S. Drug Supply Chain Security Act (DSCSA) requires every prescription drug package to have a unique serial number - like a digital fingerprint. That number is scanned at every stop: from the factory, to the distributor, to the pharmacy. If a package doesn’t match the system, it’s flagged. This system works with 99.99% accuracy. By 2023, 92% of the top 50 generic drug manufacturers had implemented full serialization. But smaller companies still lag. Why? It costs $3.5 million on average to integrate track-and-trace systems across five different platforms - from inventory software to lab equipment. That’s where Electronic Quality Management Systems (eQMS) come in. These cloud-based platforms monitor over 15,000 quality parameters per batch in real time. One quality manager at Teva said switching to eQMS cut their deviation resolution time from 14 days to under two days. But it took 18 months and $2.3 million to get it right.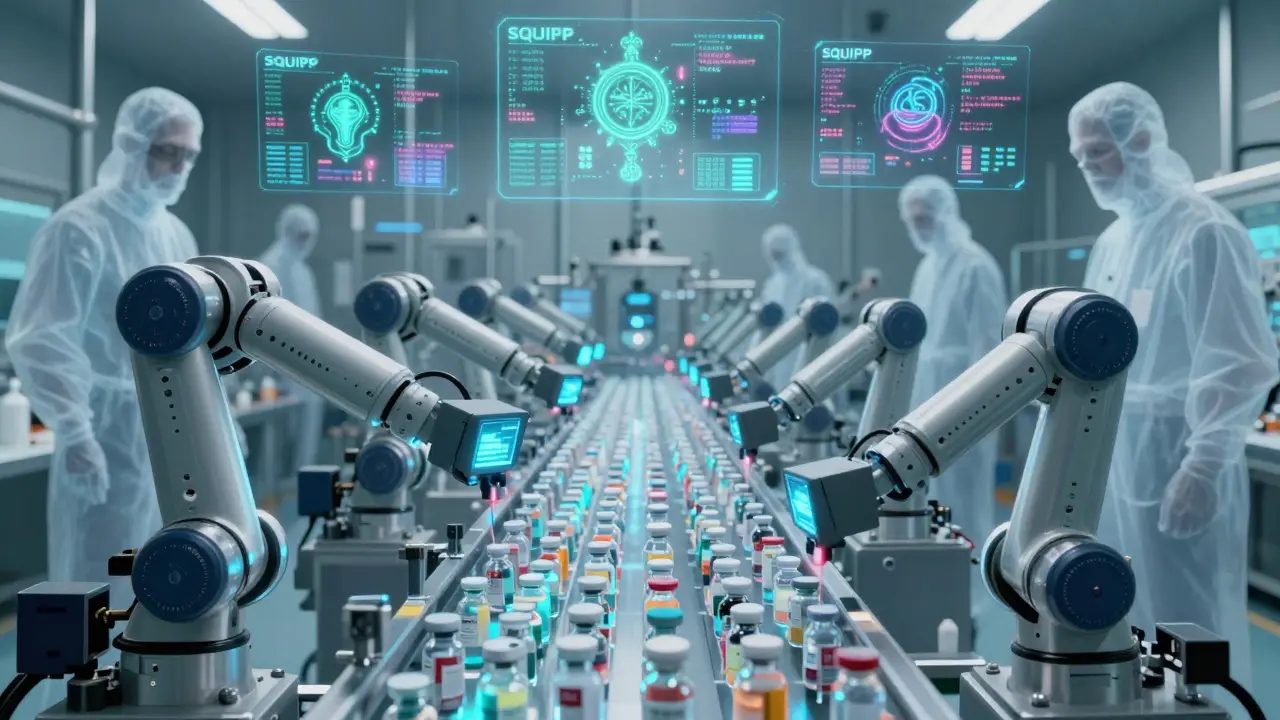
Why Generic Drugs Are Just as Safe
A common myth is that generics are lower quality. That’s not true - if they’re made under proper standards. The FDA requires generic drugs to prove they’re bioequivalent to the brand-name version. That means their absorption in the body (measured as Cmax and AUC) must fall within 80-125% of the original. That’s stricter than the 75-133% range allowed in some countries. Data backs this up. The Generic Pharmaceutical Association found that FDA-regulated generics have a 0.02% adverse event rate. Brand-name drugs? 0.03%. The difference is statistically meaningless. When quality control is done right, generics are just as safe - and far cheaper.Where the System Still Fails
Even the best systems have blind spots. The biggest risk? Polymorphs. Some drugs can exist in multiple crystal forms. One form works. Another doesn’t. It’s like having two types of sugar: one dissolves in coffee, the other doesn’t. Standard tests can’t always tell them apart. That’s how a 2018 batch of generic blood pressure pills failed - the active ingredient was correct, but the crystal structure was wrong. It didn’t dissolve properly. Patients didn’t get the dose they needed. Another problem? Global supply chains. The FDA inspects 78% of facilities in India and 65% in China. That’s lower than the 94% compliance rate in the U.S. And while the EU requires a Qualified Person (QP) to personally sign off on every batch, the U.S. relies more on process validation. That means a batch can be shipped before a human reviews it. And let’s not forget cost. A single mass spectrometer for identity testing costs $500,000 to $1 million. Many small manufacturers can’t afford it. That’s why counterfeiters target them.
What’s Next: AI, Blockchain, and Molecular Taggants
The future of quality control is smarter - and faster. The FDA is pushing for continuous manufacturing by 2025. Instead of making drugs in batches, factories will produce them nonstop, with sensors checking quality every 5 seconds. That’s real-time control, not post-production testing. The WHO is testing blockchain for antimalarial generics in Africa. Each package gets a tamper-proof digital record. Patients in rural clinics can scan a code to verify authenticity using a smartphone. Even more promising? Molecular taggants. These are tiny, invisible markers added to the drug that can be detected with a handheld device. Think of them as DNA for pills. By 2026, the EU will require quantum-resistant cryptography for serialization - meaning even hackers with quantum computers won’t be able to forge the codes. These aren’t sci-fi ideas. IBM and Siemens have invested $1.2 billion in AI-driven quality systems. Early results show AI can detect counterfeit drugs with 40% more accuracy than traditional methods.What You Can Do
As a patient, you can’t inspect a pill’s crystal structure. But you can take steps to protect yourself:- Buy from licensed pharmacies - not random websites.
- Check your prescription label. Does it match the pill? Color, shape, imprint - all should be consistent.
- If a generic looks different than usual, ask your pharmacist. It’s not a mistake - it’s a red flag.
- Report suspicious drugs to the FDA’s MedWatch program.
Quality control isn’t perfect. But it’s the only thing standing between you and a fake pill that could make you sick - or worse. The system works because it’s not about catching bad drugs. It’s about making it impossible to make them in the first place.
Are generic drugs less effective than brand-name drugs?
No, not when they’re made under proper quality control. The FDA requires generics to prove they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. Studies show they work just as well. The difference in adverse events between generics and brand-name drugs is negligible - 0.02% vs. 0.03%. The real issue is counterfeit drugs, not legitimate generics.
How can I tell if my generic drug is fake?
Look for changes in color, shape, size, or imprint on the pill. Check the packaging for misspellings, blurry printing, or missing batch numbers. Buy only from licensed pharmacies - not online vendors without a physical address. If you’re unsure, ask your pharmacist to verify the source. Legitimate manufacturers don’t change their products without notice.
Why are counterfeit drugs more common in some countries?
Countries with weak regulatory systems, poor inspection capacity, or underfunded health agencies struggle to enforce quality standards. In places where only 1 in 5 manufacturing facilities are inspected, counterfeiters thrive. The WHO estimates counterfeit drugs make up 1% of supply in developed nations but up to 30% in some developing regions. Stronger oversight, international collaboration, and technology like serialization are key to closing the gap.
Do all generic drug manufacturers follow the same rules?
In the U.S. and EU, yes - all must follow cGMP (Current Good Manufacturing Practices). But enforcement varies. The FDA inspects 94% of domestic facilities but only 78% of those in India and 65% in China. Some manufacturers cut corners to save money. That’s why regulatory agencies use risk-based inspections and require transparency in supply chains. Not every company is equal - but the standards are the same.
What’s the biggest weakness in current counterfeit detection systems?
The biggest weakness is detecting polymorphs - different crystal forms of the same chemical. A counterfeit drug can have the exact active ingredient and dosage, but if the crystal structure is wrong, it won’t dissolve properly in your body. Standard tests can’t always catch this. That’s why new technologies like near-infrared spectroscopy and molecular taggants are being developed. They look at the physical structure, not just the chemical makeup.


15 Comments
Really solid breakdown. I work in pharma logistics down here in Australia, and the SQUIPP framework is literally our bible. We’ve had batches held because a humidity sensor drifted 0.5% too high for 12 minutes. Crazy, right? But that’s how you stop a counterfeit from slipping through. Quality isn’t a checkpoint-it’s the whole damn road.
Oh please. You think all this ‘quality control’ nonsense actually works? The FDA approves generics from factories that haven’t been inspected in 7 years. And don’t get me started on India. They’re literally printing pills in basements and shipping them under ‘FDA-compliant’ labels. This whole system is a corporate shell game. You’re just being sold a lie wrapped in HPLC reports.
While the article presents a compelling case for standardized quality control, it is worth noting that the implementation of eQMS and serialization technologies is not universally accessible. Small manufacturers, particularly in developing economies, face significant capital constraints. A purely technological solution may inadvertently create a two-tiered system where only large corporations can guarantee safety. Regulatory harmonization and public-private funding initiatives are necessary to prevent this disparity.
OMG this is so important!! I just found out my blood pressure med looked different and I was about to panic until my pharmacist said it’s a new batch-same formula, different dye. THANK YOU for explaining why that’s totally fine. People need to chill and trust the system. Also-SCAN YOUR CODES. It’s like 2 seconds on your phone. Do it.
Bro. I work in a pharmacy. Last week, someone brought in a bottle of generic metformin that had a weird smell. We flagged it. Turned out the binder was laced with a solvent from a Chinese supplier. FDA didn’t catch it. We did. And now? They’re shutting down the whole line. So yeah, tech helps-but people still matter. 🤝🧪
Yesss this is why I always ask my pharmacist if the generic is from the same manufacturer as last time. I don’t care if it’s cheaper if I feel weird after taking it. One time I got a different batch and my headaches got worse. Turned out the coating was off. Not the drug-just the damn tablet. Quality control isn’t sexy but it’s everything.
Imagine if every pill had its own little digital tattoo. That’s what molecular taggants are-tiny, invisible DNA-like markers you can scan with a phone. It’s like giving each pill a passport. And AI? It’s learning to spot fake crystal structures by how the light bounces off them. We’re not just catching bad drugs anymore-we’re making it impossible to make them. This isn’t the future. It’s happening right now.
Let’s be honest: this entire article is corporate propaganda. The FDA is a revolving door for pharma executives. The ‘0.02% adverse event rate’? That’s self-reported. They don’t track long-term effects. And polymorphs? They’ve known about this for decades. They just don’t want to admit it because fixing it would cost too much. You think they care about you? They care about liability.
India make good generic, but some factory no have money for machine. So they use old way. I know one guy, his brother work in factory, they use same powder but mix with different binder. No one check. Just luck if work. Sad but true.
So you’re telling me the government and big pharma are working together to protect us? Right. Next you’ll say the moon landing wasn’t faked. All this ‘quality control’ is just a smokescreen. The real goal is to lock out competition so brand-name drugs stay at $500 a pill while generics cost $2. This whole thing is a monopoly dressed up as safety.
I’ve been on generics for 12 years. Never had an issue. But I get why people worry. I had a friend who got a bad batch from a shady online pharmacy-she ended up in the ER. It wasn’t the drug. It was the source. That’s why I only ever refill at my local pharmacy. It’s not about trust in the system-it’s about knowing where your medicine comes from. Small steps matter.
Wait, so you’re saying the FDA doesn’t inspect every single batch? But I thought they were the gold standard? This makes me feel way less safe. I’m switching back to brand-name. Even if it costs 10x more. At least I know who made it.
They’re lying. The real reason they don’t test for polymorphs is because it would expose how many generics are just sugar pills with the right chemical name. The system is rigged. I read a whistleblower report that said 37% of Indian-manufactured generics have inactive forms. They’re selling placebos. And the FDA? They’re paid off. Wake up, sheeple.
Why are we even talking about this? It’s 2024. You can’t trust anything anymore. The pills are being 3D printed in China and shipped via Amazon. Your ‘quality control’ is a joke. I don’t take generics anymore. I buy from Canada. At least there’s some oversight there.
This was so helpful. I used to think generics were just cheap knockoffs. Now I get it-they’re the same drug, just made better. The real villains are the shady online sellers and the companies cutting corners. Let’s support the good manufacturers. They’re doing the hard work so we don’t have to worry. Cheers to quality!