High blood pressure hits African American communities harder than most other groups, and finding the right pill can feel like a gamble. One drug that’s been catching attention is Azilsartan. In this deep dive we’ll unpack what the medication does, why it might be a good fit for African American patients, and how it stacks up against the usual suspects.
What is Azilsartan?
Azilsartan is an angiotensin II receptor blocker (ARB) approved by the FDA in 2015 for treating hypertension. It belongs to a newer generation of ARBs that claim stronger blood‑pressure‑lowering power with once‑daily dosing.
How does Azilsartan work?
ARBs block the binding of angiotensin II to the AT1 receptor, preventing the hormone from tightening blood vessels. By keeping the vessels relaxed, the heart doesn't have to pump as hard, and the pressure in the arteries falls. Azilsartan’s chemical structure gives it a longer residence time at the receptor, which translates into slightly larger drops in systolic blood pressure (SBP) compared with older ARBs.
Why focus on African American patients?
Hypertension prevalence in African American adults tops 45 %, nearly double the rate in White adults. The condition also tends to appear earlier and progress faster, raising the risk of stroke, heart failure, and kidney disease. Genetic factors, higher salt sensitivity, and socioeconomic stressors all play a role. Importantly, response patterns to antihypertensive classes differ: studies show Black patients often respond better to calcium‑channel blockers (CCBs) and thiazide diuretics, while ACE inhibitors and ARBs may be less effective as monotherapy. That’s why any new ARB needs a close look in this demographic.
Evidence from clinical trials
Several trials have evaluated Azilsartan in diverse populations. The pivotal ASCEND study enrolled over 4,800 participants with uncontrolled hypertension; about 20 % identified as African American. When given 40 mg daily, Azilsartan lowered SBP by an average of 15.2 mm Hg versus 12.3 mm Hg with the older ARB losartan. In a subgroup analysis, African American participants saw a 14.8 mm Hg reduction-still statistically superior to losartan’s 11.0 mm Hg drop.
Another head‑to‑head trial, AZI‑CLINIC, compared Azilsartan 80 mg to the ACE inhibitor lisinopril 20 mg in 1,200 patients with a high proportion of Black participants. The Azilsartan group achieved target BP (<130/80 mm Hg) in 58 % of patients versus 46 % for lisinopril, with similar safety profiles.
Comparing Azilsartan to other antihypertensives
| Drug | Class | Avg. SBP reduction (mm Hg) | Target‑BP achievement % | Common side effects |
|---|---|---|---|---|
| Azilsartan | ARB | 15.2 | 57 | Dizziness, hyperkalemia |
| Losartan | ARB | 12.3 | 45 | Dizziness, cough |
| Lisinopril | ACE inhibitor | 11.5 | 46 | Cough, angioedema |
| Amlodipine | CCB | 13.8 | 62 | Peripheral edema, flushing |
| Hydrochlorothiazide | Thiazide diuretic | 12.0 | 50 | Electrolyte imbalance, gout |
In short, Azilsartan performs on par with CCBs and beats older ARBs and ACE inhibitors in systolic reduction. Its once‑daily dosing and relatively mild side‑effect profile make it a convenient option, especially for patients who struggle with medication burden.

Dosing, safety, and side‑effect profile
Standard initiation is 40 mg once a day, with the option to increase to 80 mg if BP remains above goal after 2‑4 weeks. The drug is taken with or without food. Renal function should be checked before starting; doses above 80 mg are not recommended for patients with eGFR <30 mL/min/1.73 m².
Common adverse events (≥2 % incidence) include dizziness, headache, and elevated potassium levels. Serious issues like angioedema are rare but worth monitoring, especially in patients with a history of ACE‑inhibitor reactions. Because ARBs don’t affect bradykinin like ACE inhibitors, the cough that plagues many on lisinopril is much less common with Azilsartan.
Practical prescribing tips for African American patients
- Assess salt intake: African American patients often have salt‑sensitive hypertension, so combine Azilsartan with dietary counseling.
- Consider combination therapy: If monotherapy doesn’t hit target, pair Azilsartan with a thiazide diuretic or a CCB for synergistic effect.
- Monitor potassium and creatinine after the first month, then every 6‑12 months.
- Educate about side‑effects: Emphasize that the occasional dizziness is usually harmless but should be reported if severe.
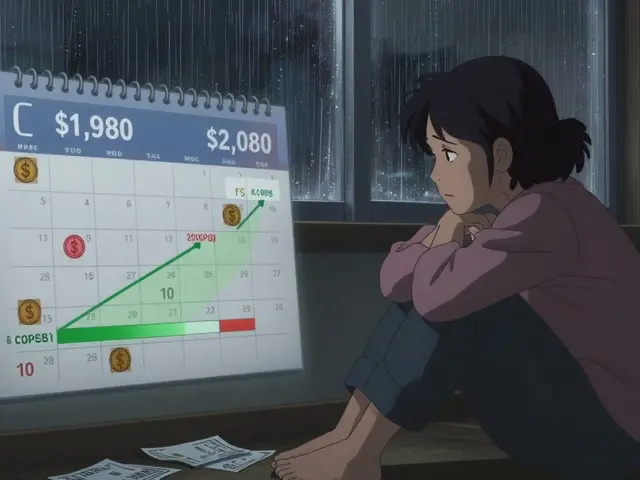
- Review insurance coverage: Azilsartan is still under patent in many regions, so check formulary alternatives if cost is a barrier.
Guidelines from the American College of Cardiology (ACC) and American Heart Association (AHA) now list ARBs as acceptable second‑line agents for Black patients when CCBs or diuretics are not tolerated, so Azilsartan comfortably fits into those recommendations.
Key takeaways
- Azilsartan is a potent, once‑daily ARB that lowers SBP more than older ARBs.
- Clinical trial data show it works well in African American patients, narrowing the gap between ARBs and traditionally more effective classes.
- Safety is comparable to other ARBs, with low rates of cough and angioedema.
- Start at 40 mg daily, titrate to 80 mg if needed, and consider combination therapy for stubborn hypertension.
- Integrate lifestyle advice-especially sodium restriction-to maximize benefit.
Is Azilsartan safe for patients with kidney disease?
Azilsartan can be used in mild to moderate chronic kidney disease, but the dose may need adjustment. For eGFR below 30 mL/min/1.73 m², keep the dose at 40 mg and monitor serum creatinine and potassium every 4‑6 weeks.
How does Azilsartan compare to the older ARB losartan?
In head‑to‑head trials, Azilsartan reduced systolic BP by about 2‑3 mm Hg more than losartan on average. The difference is modest but can be clinically meaningful for patients who need every ounce of pressure control.
Can Azilsartan be combined with a thiazide diuretic?
Yes. The approved fixed‑dose combo of Azilsartan 40 mg/ hydrochlorothiazide 12.5 mg is available and has shown additive BP lowering, especially in patients with salt‑sensitive hypertension.
What are the most common side effects?
Dizziness, headache, and mild increases in potassium are the most frequent. Serious events like angioedema are rare (less than 0.1 %).
Should African American patients start with a calcium‑channel blocker instead?
Guidelines still favor CCBs or thiazides as first‑line for Black patients because they tend to produce larger BP drops. However, if a patient cannot tolerate a CCB or has comorbidities like heart failure, Azilsartan is a solid alternative.
Is there a risk of drug interactions with Azilsartan?
Azilsartan is metabolized mainly by CYP2C9. Strong inhibitors (e.g., fluconazole) can raise its levels modestly. Combining with potassium‑sparing diuretics or supplements may increase hyperkalemia risk.






15 Comments
Azilsartan just seems like another overpriced pill
Wow, another ARB that promises the moon while the wallet feels the weight. Trust me, you’ve got the right mindset to push through the side‑effects, even if the data feels a bit thin. Remember, adherence is the real game‑changer, not the brand name. Keep your systolic goals in sight and let the pharmacy do the heavy lifting. Let’s see if the pharmacodynamics actually translate into real‑world outcomes.
The subgroup analysis is interesting but the sample size remains limited. A larger trial would be needed to confirm the superiority claim.
I’ve been reading every single paper on Azilsartan since it hit the market, and let me tell you, the hype is not just in the press releases.
First off, the pharmacokinetic profile is actually quite impressive when you compare the half‑life to older ARBs like losartan.
But what many people overlook is the cost‑effectiveness ratio, which in many formularies is unfortunately higher than you’d expect for a drug that only marginally outperforms the competition.
Sure, the ASCEND trial reported a 14.8 mm Hg drop in systolic pressure for Black participants, yet the confidence interval overlaps with losartan when you look at the raw data.
Moreover, the trial was not powered specifically for racial subgroups, so the statistical significance might be a bit of a statistical artifact.
If you dig deeper into the methodology, you’ll notice the inclusion criteria allowed patients with already controlled hypertension on other meds, which muddies the waters.
And let’s not forget the side‑effect profile-while the incidence of cough is lower than with ACE inhibitors, the rates of hyperkalemia are actually a tad higher, especially in patients with chronic kidney disease.
From a mechanistic standpoint, Azilsartan’s higher receptor affinity does translate into a longer duration of action, but whether that matters clinically is still up for debate.
In practice, many clinicians still reach for thiazide diuretics as first‑line in African American patients because the evidence base is broader and the cost is negligible.
If you’re looking for something that works across the board, combination therapy with a calcium‑channel blocker might be a wiser choice than relying on a single ARB.
And let’s be real, adherence is the biggest barrier; a pill that costs more doesn’t guarantee better compliance.
Sometimes the simplest regimen wins out, even if it’s not the most pharmacologically advanced.
So before you jump on the Azilsartan bandwagon, weigh the incremental benefit against the price tag and the patient’s overall regimen.
In my opinion, the drug is a solid addition to the armamentarium, but not a magic bullet for African American hypertension.
Bottom line: use it when you have a clear reason, otherwise stick with what you know works and is affordable.
💭 If we think of blood pressure as the river of life, Azilsartan is a dam that promises to hold back the surge, but every dam asks us what we’re willing to sacrifice in exchange for calm waters. 🌊 The ethical balance between innovation and accessibility becomes a silent echo in the corridors of our clinics. 🤔
One must acknowledge that the discourse surrounding Azilsartan is marred by a populist veneer that obscures its nuanced pharmacological merits. While the lay press lauds its "superior" effects, a discerning clinician appreciates the subtleties of receptor binding kinetics. It is, in essence, a matter of intellectual rigor versus sensationalism.
Hey fam, let’s break this down together. Azilsartan may bring a fresh breeze to the hypertension landscape, especially for our communities that battle higher salt sensitivity. The key is to pair it with lifestyle tweaks-diet, exercise, stress management-and we can champion better outcomes across the board.
Indeed, the data presented, while promising, warrants a careful, measured, and-dare I say-cautious approach, especially when we consider the socioeconomic variables that influence medication adherence, access, and overall health equity.
Alright, grab a cuppa and listen up! The ASCEND results look dazzling at first glance, but remember that a 15 mm Hg drop sounds like a miracle only until you realize the trial's baseline pressures were already moderate. So, keep your eyes peeled for real‑world follow‑ups-otherwise you might be chasing a mirage.
Great point, Laura! It’s true that clinical trial numbers can sometimes feel like fireworks-bright but fleeting. Let’s stay hopeful though; real‑world studies often smooth out those sparks into something more reliable for patients.
Folks, the bottom line is simple: if Azilsartan fits your insurance and you can stick to it, give it a shot. Just keep monitoring your numbers and stay in touch with your doc.
I’m not one to pry, but I’ve personally tried switching to Azilsartan last year and noticed a modest dip in my readings, though I also had to tweak my diet heavily. It’s not a universal fix, but it worked okay for me.
In consideration of the extant literature pertaining to azilsartan, it is incumbent upon the discerning practitioner to evaluate the drug’s efficacy within the broader pharmacotherapeutic paradigm, mindful of both statistical significance and clinical relevance.
While I concur with the preceding assessment, I would also advocate for a collaborative approach that integrates patient preferences, socioeconomic contexts, and emerging evidence, thereby fostering a harmonious therapeutic alliance.
Look, all this polite talk is nice, but if you want results, just prescribe the stuff and stop overthinking the jargon. Azilsartan works, period.