Phosphate Binders: What They Are, How They Work, and What You Need to Know
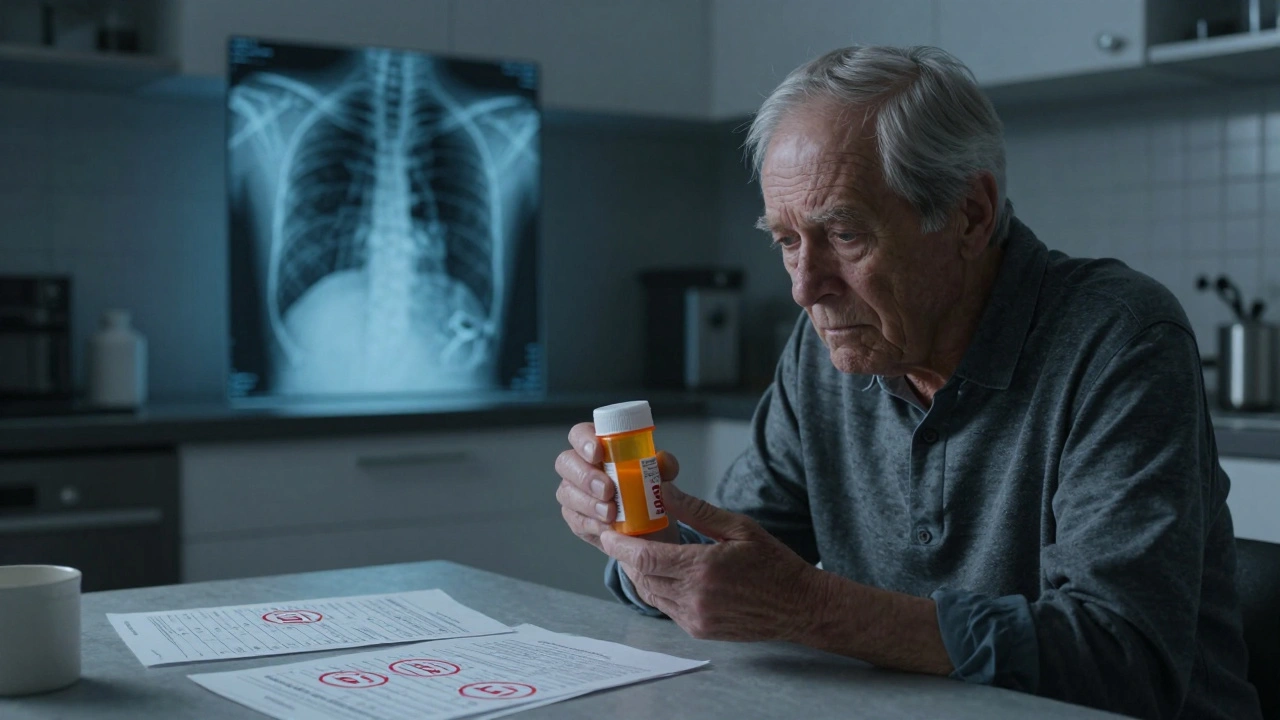
When your kidneys can’t filter phosphorus properly, it builds up in your blood — a condition called hyperphosphatemia, a dangerous elevation of phosphate levels in the blood, often linked to chronic kidney disease. Also known as high blood phosphorus, it’s not just a lab number — it’s a silent threat to your heart, bones, and blood vessels. That’s where phosphate binders, medications taken with meals to block phosphorus absorption from food. These aren’t vitamins or supplements — they’re prescription drugs designed to bind to phosphorus in your gut so your body can’t absorb it. Without them, even healthy foods like dairy, nuts, and meats can become dangerous.
Most people on dialysis, a treatment that replaces kidney function when they fail. Also known as renal replacement therapy, it’s a lifeline — but it doesn’t fully remove phosphorus. need phosphate binders because dialysis alone can’t keep up. The two main types are calcium-based binders like calcium carbonate and calcium acetate, and non-calcium options like sevelamer and lanthanum. Calcium binders are cheaper but can cause too much calcium in your blood, leading to calcification in your arteries. Non-calcium ones avoid that risk but cost more. Then there’s iron-based binders — newer, less common, but useful if you’re also anemic.
It’s not just about popping pills. Timing matters — you have to take them with every meal or they won’t work. Skip one bite, and phosphorus slips through. Many patients struggle with side effects: nausea, constipation, or stomach upset. That’s why switching binders is common. Your doctor might try one, see how your phosphorus levels respond, then adjust. It’s trial and error, but it’s critical. High phosphorus doesn’t just hurt your kidneys — it stiffens your heart valves, weakens your bones, and raises your risk of death.
What you eat also plays a role. Even with binders, eating too many high-phosphorus foods makes your job harder. Processed foods, colas, and packaged snacks are full of hidden phosphorus additives — and they’re not listed on labels as "phosphorus." You can’t always trust "no added phosphate" claims. That’s why dietitians are part of the team. They help you find safe protein sources, swap out soda for water, and make meals that don’t sabotage your meds.
And it’s not just for dialysis patients. People with advanced kidney disease who aren’t on dialysis yet also need binders to slow damage. Even if you feel fine, high phosphorus is working under the surface. That’s why regular blood tests — checking phosphorus, calcium, and PTH — are non-negotiable. One number can tell you if your binder is working, if your dose needs tweaking, or if you’re slipping back into danger.
Below, you’ll find real-world stories and science-backed guides on how phosphate binders fit into broader medication safety. From how they interact with other drugs like vitamin D and iron supplements, to why some people get confused about when to take them, to how generic versions compare — this collection cuts through the noise. You’ll learn what works, what doesn’t, and how to talk to your doctor about the right choice for your body.
Antacids and Kidney Disease: What You Need to Know About Phosphate Binders and Risks
Antacids like Tums and Milk of Magnesia can be dangerous for people with kidney disease. Learn how calcium, aluminum, and magnesium in these meds affect phosphate levels, heart health, and kidney function - and what safer options exist.
read more




