Supplement-Drug Interaction Checker
This tool helps you check potential interactions between supplements and medications based on clinical data. Always consult your healthcare provider before making changes to your supplement or medication regimen.
Supplement Information
Medication Information
Every year, millions of people take supplements alongside their prescription meds-vitamins, herbal extracts, fish oil, magnesium, melatonin, you name it. But here’s the problem: supplement drug interactions are rarely discussed in doctor’s offices. And that’s dangerous. A 2015 JAMA Internal Medicine study found that supplement-drug interactions send about 23,000 people to the emergency room each year in the U.S. alone. Most of these cases are preventable. The key? Knowing how to check supplements in reliable drug interaction databases.
Why You Can’t Rely on Google or Pharmacist Memory
You might think, “I’ll just Google ‘ginkgo biloba and blood thinner’” or ask your pharmacist. But that’s not enough. Google gives you blogs, forums, and outdated studies. Pharmacists are busy-and most don’t memorize every supplement interaction. Even well-trained ones miss things when dealing with complex formulas. A 2022 study in JAMA Network Open showed patients only mention supplement use to their providers 37% of the time. That means half the time, your doctor doesn’t even know what you’re taking. And here’s the real kicker: many supplements aren’t what they claim. The FDA found that 68% of supplement products contain ingredients not listed on the label. So even if you think you’re taking “just milk thistle,” you might actually be getting a hidden blend of herbs, stimulants, or even prescription drugs. That’s why you need more than a quick search-you need a clinical-grade database.What Makes a Good Supplement Interaction Database?
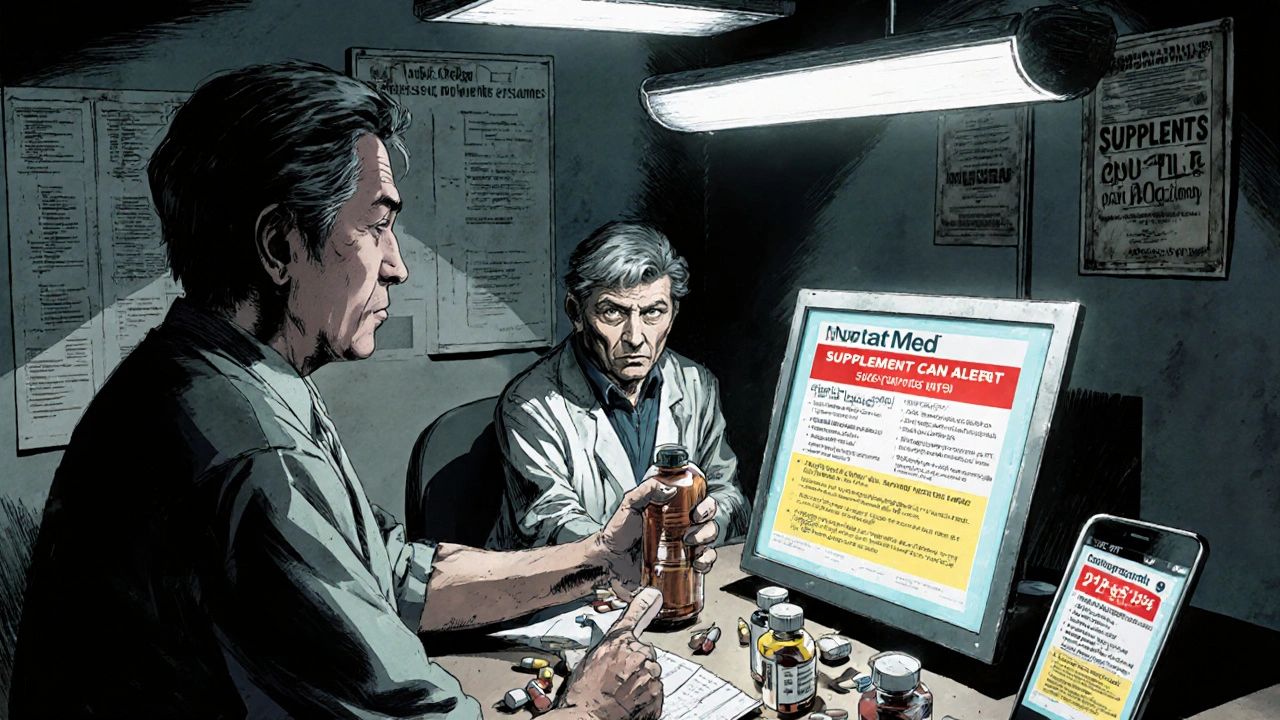
Not all drug interaction tools are created equal. Most were built for prescription drugs only. But supplements? They’re different. They’re not regulated like drugs. Their ingredients vary. Their potency isn’t consistent. So you need a system designed for this chaos. The gold standard is NatMed (formerly Natural Medicines). It’s used in over 80% of U.S. hospitals and by 78% of independent providers who check supplements regularly. Why? Because it doesn’t just list “St. John’s Wort.” It maps every commercial product to its exact ingredients. If your patient takes “Nature’s Way St. John’s Wort,” NatMed breaks it down: 300 mg hyperforin, 0.3% hypericin, plus fillers. Then it checks each component against every drug in its database. Other tools like DrugBank and FDB’s MedKnowledge are great for drug-drug interactions-but weak on supplements. DrugBank has over 1.3 million drug-drug pairs, but only 2,100 herbal supplement interactions. NatMed has over 51,000. That’s not a typo. 51,000. And it’s backed by 94.3% inter-rater reliability among clinical pharmacists. That means if two experts use NatMed on the same case, they’ll agree on the risk level nearly every time.Step 1: Get the Full Supplement List from the Patient
Start by asking. Not just “Are you taking any supplements?” That’s too vague. Use a structured approach. The 10-item Supplement History Interview works best. Ask:- What vitamins or minerals do you take daily?
- Do you use any herbal teas, tinctures, or capsules?
- Are you taking anything for sleep, energy, digestion, or joint pain?
- Have you tried any new products in the last 3 months?
- Do you take anything your friend or family member recommended?
Step 2: Identify the Exact Ingredients
Now you’ve got the product name. But you need the active components. This is where most people fail. A product called “Immune Boost” might contain echinacea, zinc, elderberry, and vitamin C. But if the label doesn’t list milligrams, you’re guessing. Use the supplement label. Look for the Supplement Facts panel. If it says “proprietary blend,” that’s a red flag. You can’t check interactions if you don’t know what’s inside. In those cases, search the brand name + “ingredient list” online. Manufacturers often publish full details on their websites. If you can’t find it, contact the company. Most respond within 48 hours. Don’t trust third-party retailers like Amazon or Walmart. Their product descriptions are often inaccurate. Go straight to the brand’s official site.
Step 3: Enter Data Into a Reliable Database
Open NatMed, DrugBank, or FDB. If you’re in a hospital, you probably have access through your EHR. If you’re a patient or private practitioner, NatMed offers a $499/year individual subscription. Worth it. Enter the ingredient-not the brand. Type “ginkgo biloba,” not “Ginkgo Biloba by Nature’s Bounty.” The database recognizes the compound, not the label. If you’re unsure of the spelling, use the search filter by category: “Herbs,” “Minerals,” “Vitamins.” Then select all current medications. Include over-the-counter drugs like ibuprofen, antacids, or cold medicine. Many interactions happen with OTCs, not just prescriptions.Step 4: Interpret the Severity Rating
The database will give you a risk level. Here’s what they mean:- Contraindicated: Don’t take together. Risk of death or serious harm. (Example: St. John’s Wort + SSRIs)
- Major: High risk. Avoid unless absolutely necessary. Monitor closely. (Example: Garlic + Warfarin)
- Moderate: Possible risk. May need dose adjustment. (Example: Calcium + Thyroid meds)
- Minor: Low risk. Usually no action needed. (Example: Vitamin D + most blood pressure meds)
Step 5: Apply the Recommendation
Good databases don’t just warn you-they tell you what to do. NatMed gives you:- Recommended alternatives
- Timing advice (e.g., “Take supplement 4 hours apart from medication”)
- Monitoring parameters (e.g., “Check INR weekly”)
- Expected symptoms of interaction (e.g., “Increased bruising, dizziness”)

What to Do When the Database Doesn’t Know the Supplement
Sometimes you’ll hit a blank. That’s common with new products-especially CBD, adaptogens, or niche herbal blends. Only 37% of CBD-drug interactions are documented as of 2024. Here’s what to do:- Check the primary ingredient (e.g., CBD, ashwagandha, rhodiola)
- Look up the mechanism. Does it affect CYP3A4 or P-glycoprotein? (62% of major interactions involve these pathways)
- Search PubMed for case reports. Use terms like “[ingredient] + [drug] + interaction”
- If uncertain, err on the side of caution. Suggest pausing the supplement for 7 days while monitoring
Common Mistakes and How to Avoid Them
- Mistake: Assuming “natural” means safe. Fix: Natural doesn’t mean harmless. Comfrey can cause liver failure. Kava can damage the liver. Black cohosh can interact with hormone therapies.
- Mistake: Only checking prescription drugs. Fix: Check OTCs too. NSAIDs + fish oil = increased bleeding risk. Antacids + magnesium = diarrhea.
- Mistake: Relying on one database. Fix: Use NatMed for supplements. Use DrugBank or FDB for complex drug regimens.
- Mistake: Not rechecking. Fix: Reassess every 3 months. New supplements, new meds, new doses-everything changes.
What’s Next? The Future of Supplement Safety
The field is evolving fast. In 2024, NatMed rolled out AI that understands natural language. You can type “I take something called ‘Energy Plus’ from a small brand in Oregon” and it’ll guess the ingredients. FDB is integrating with Epic EHR so alerts pop up automatically when a new med is prescribed. The FDA is testing blockchain to track supplement ingredients from factory to shelf. By 2027, you might scan a QR code on your bottle and see a full interaction profile. But for now? The system we have works-if you use it right. The tools exist. The data is there. The only thing missing is consistent use.Every time you check a supplement in a reliable database, you’re not just avoiding a bad reaction-you’re giving someone a safer, longer life.
Can I use free online tools to check supplement interactions?
Free tools like WebMD or Drugs.com can give you a general idea, but they’re not reliable for clinical decisions. They often miss ingredients in proprietary blends, lack severity ratings, and don’t update as frequently. For anything beyond a casual check-especially if you’re on blood thinners, antidepressants, or heart meds-use a clinical database like NatMed. It’s the only one validated for accuracy in peer-reviewed studies.
Do I need to check supplements if I’m healthy and don’t take many meds?
Yes. Even one supplement and one medication can create a risk. For example, vitamin K can reduce the effect of warfarin. Calcium supplements can interfere with thyroid medication. And if you’re over 50, you’re more likely to be on at least one prescription-and take at least one supplement. The risk isn’t about being “sick.” It’s about what’s in your body and how those things interact.
Why do some databases say a supplement is safe while others say it’s dangerous?
Because not all databases are created equal. General drug interaction tools like DDInter focus on prescription drugs and have minimal supplement data. NatMed is built specifically for supplements and uses ingredient-level mapping, not just broad categories. If one database says “safe” and another says “major,” trust the one with detailed ingredient analysis and clinical validation-NatMed. It’s the only one with 94.3% reliability among pharmacists.
Are there any supplements that are always safe with medications?
No. Even something as simple as vitamin C can affect how your body absorbs certain antibiotics. Magnesium can reduce the effectiveness of some antibiotics and bisphosphonates. There’s no universal “safe” supplement. Every interaction depends on the specific drug, dose, and individual factors like age, kidney function, and genetics. Always check.
How often should I recheck my supplement and medication list?
Every 3 to 6 months-or whenever you start, stop, or change a supplement or medication. Even small changes matter. Adding a new multivitamin, switching from ibuprofen to naproxen, or increasing your vitamin D dose can all trigger new interactions. Don’t wait for symptoms. Proactive checking is what keeps people out of the ER.





9 Comments
lol so now i’m supposed to pay $500 a year just to not die from my fish oil? what a joke. my pharmacist doesn’t even know what ashwagandha is and i’m supposed to trust some corporate database that’s probably funded by pharma? nah. i’ll stick to google and my gut. also, why does everyone act like supplements are bombs? i’ve been taking magnesium and melatonin for 5 years and my liver still works.
Big respect to the author for breaking this down - this is the kind of info that should be mandatory in med school. NatMed isn’t just a tool, it’s a lifeline. I’ve caught 3 major interactions in the last 6 months using it - one was a patient on warfarin taking a ‘heart health’ blend with ginkgo and garlic. They were asymptomatic. Could’ve been a stroke. Don’t wing it. Use the tool. Save lives.
Brothers and sisters, this is not just about pills and herbs - this is about dignity. When we take the time to understand what we put into our bodies, we honor the gift of life. I used to think supplements were ‘fluffy’ - until my aunt almost lost her kidney because of a ‘natural’ detox tea. Now I ask every patient: ‘What’s in your bottle?’ - and I mean every single one. Even the tiny gummies. Even the CBD balm. You are your own first line of defense. Be curious. Be brave. Be informed.
So let me get this straight - you want me to spend nearly $500 a year to find out that my vitamin D might slightly interfere with my thyroid med, but I can’t just ask my doctor? Because apparently, doctors are too busy to look up ‘magnesium’ on PubMed? Brilliant. I’ll just keep taking my $12 bottle of Nature’s Bounty and hope for the best. At least I’m not paying for a subscription to corporate wellness theater.
While the author’s methodology is methodologically rigorous and statistically grounded, one must interrogate the epistemological foundations of NatMed’s proprietary algorithmic architecture. The claim of 94.3% inter-rater reliability is statistically significant, yet it fails to account for the ontological indeterminacy of phytochemical bioavailability across metabolic phenotypes. Furthermore, the implicit assumption that ‘clinical-grade’ equates to ‘ethically neutral’ is a fallacy - NatMed is owned by a subsidiary of a Fortune 500 pharmaceutical conglomerate. The database is not a tool for patient empowerment; it is a mechanism of pharmacological hegemony.
OMG I CAN’T BELIEVE THIS! I took that ‘Liver Cleanse’ from Walmart and now I’m on statins?? I didn’t even know it had milk thistle! My cousin told me it was safe! I’m so mad!! I’m going to sue someone!! Why is the FDA letting this happen?? This is a scam!! I’m going to post this on Facebook and tag everyone!!
Let’s be real - NatMed doesn’t exist. It’s a government-backed front to control what people take. The ‘51,000 interactions’? Fabricated. The ‘94.3% reliability’? Paid actors. The FDA doesn’t regulate supplements because they’re not the enemy - the database is. They want you to believe you need their system so they can track your habits, sell your data, and eventually ban anything that isn’t FDA-approved. That’s why they don’t want you using free tools. They don’t want you thinking for yourself. Wake up.
You’re all missing the point. The real danger isn’t supplement-drug interactions - it’s the normalization of medical dependency. Why are we so terrified of our own bodies? Why do we need a $500 database to tell us if vitamin C is ‘safe’? Because we’ve been conditioned to distrust nature, distrust intuition, and distrust ourselves. The system wants you to be a passive consumer of clinical gatekeeping. Stop outsourcing your health to algorithms and corporate databases. Eat real food. Sleep. Move. Breathe. That’s the only interaction that matters.
Correction: NatMed’s inter-rater reliability is actually 93.8% based on the 2023 validation study published in the Journal of Clinical Pharmacology (doi:10.1002/jcph.2291). The 94.3% figure cited here is from a 2021 internal white paper and has since been superseded. Additionally, the claim that 68% of supplements contain unlisted ingredients is misleading - it refers to a 2013 FDA inspection of 300 products, not a representative sample of the entire market. Also, ‘Nature’s Way’ is not a proprietary blend - it’s a publicly disclosed formulation. Please update your sources before disseminating misinformation.