ACTH Test Results Calculator
This tool determines if your adrenal function is ready to resume natural cortisol production based on the 2024 Endocrine Society guidelines. Enter your test results to see your next steps.
ACTH Test Results
Tapering Guidance
Note: This tool follows 2024 Endocrine Society guidelines. Always work with your doctor to adjust your taper.
Stopping long-term steroid use isn’t as simple as just cutting the pills. If you’ve been on prednisone, hydrocortisone, or another glucocorticoid for months-or years-your body has stopped making its own cortisol. Your adrenal glands have gone quiet. Suddenly stopping steroids can trigger a life-threatening crash called adrenal crisis. That’s where ACTH stimulation testing comes in. It’s not optional. It’s the gold standard for knowing when your body is ready to wake up its own cortisol production.
Why Your Adrenals Shut Down
When you take steroids for more than a few weeks, your brain gets the message: "We’ve got plenty of cortisol already." So it turns off the signal to your adrenal glands. This is called HPA axis suppression. It’s not a glitch-it’s normal physiology. But when you stop the pills, your adrenals don’t just snap back to life. They need time. And if you rush the process, your body has nothing left to fight off stress.Think of it like a car that’s been parked for six months. You don’t just turn the key and expect it to roar. You check the battery, the fuel, the oil. ACTH testing is the diagnostic check-up for your adrenal system.
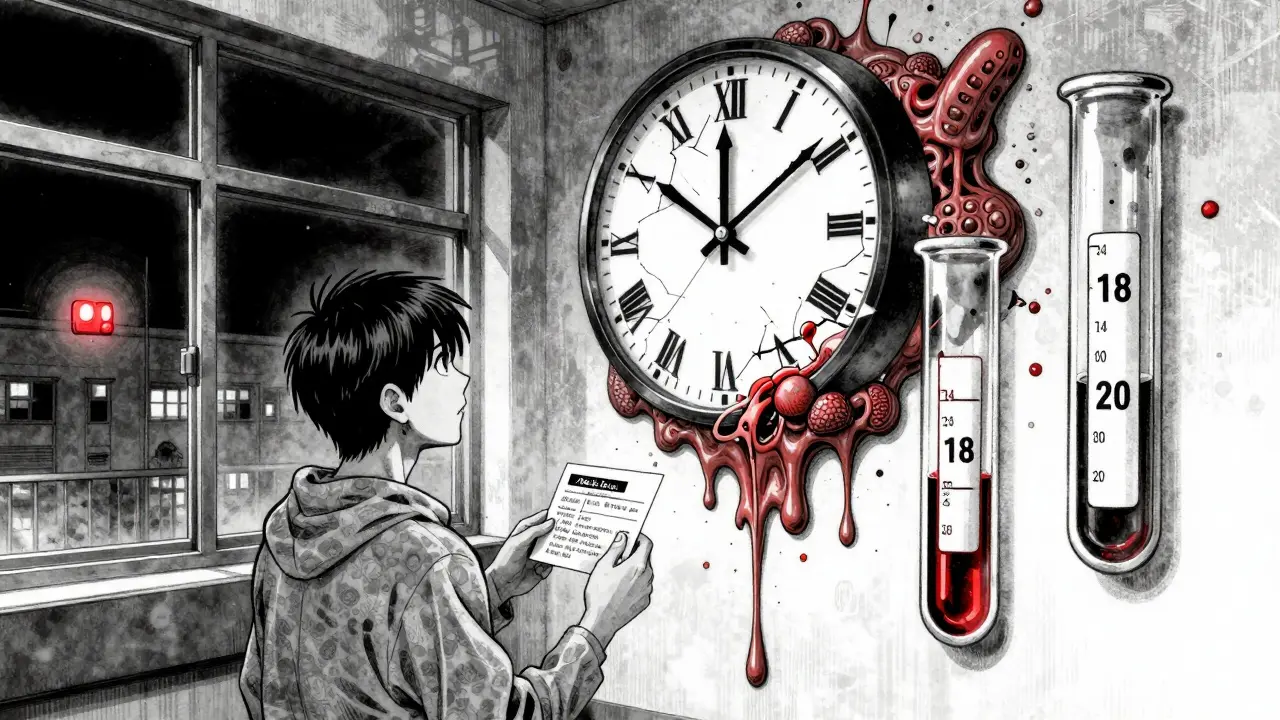
What Is an ACTH Stimulation Test?
The test is simple, but precise. You get a 250 mcg shot of synthetic ACTH-called cosyntropin-either into your muscle or vein. Then, blood is drawn at 0, 30, and 60 minutes to measure your cortisol levels. The goal? To see if your adrenals can respond.The current standard, set by the Endocrine Society and European Society of Endocrinology in their June 2024 joint guideline, says a peak cortisol level of 18-20 mcg/dL or higher means your adrenals are working. Below 14 mcg/dL? You still need replacement steroids. Between 14 and 18? It’s a gray zone-you might need more time, or another test.
This isn’t a one-time test. It’s done at key points during your taper. Usually, when you’ve reached the lowest replacement dose-about 4-6 mg of prednisone per day-and you’re preparing to stop completely.
How Fast Should You Taper?
There’s no one-size-fits-all schedule. But the rules are clear: the longer you were on steroids, the slower you go.- If you were on steroids for 3-12 months, drop by 2.5-5 mg of prednisone every 1-2 weeks until you hit 10-15 mg/day. Then cut by 20-25% per week.
- If you were on them for more than a year, recovery takes about one month for every month you were on steroids. That means a 2-year course could mean 18-24 months of careful tapering.
The PJ Nicholoff Protocol, used widely for patients with Duchenne muscular dystrophy, breaks this down into 14 detailed steps. It’s not just about the numbers-it’s about watching for muscle weakness, fatigue, or flare-ups of the original condition. If symptoms return, you might need to pause the taper and go back to the last tolerated dose.
When to Test-and When Not To
The 2024 guidelines are clear: if you’ve been on steroids for less than 3-4 weeks, you likely don’t need testing. Your adrenals haven’t had time to shut down. But if you’ve been on them longer? Test.Here’s the debate: Should everyone get tested? The Endocrine Society says only if you have symptoms or are high-risk. But other experts, like Dr. Alessandro Prete, argue that routine testing at the 6-month mark prevents 92% of adrenal crises. In real-world practice, many patients don’t feel symptoms until it’s too late. Fatigue, nausea, dizziness-these are easy to blame on stress, aging, or the original illness. But they could be your body screaming for cortisol.
That’s why clinics with structured testing programs see adrenal crisis rates drop from 8.5% to just 1.2%. That’s an 86% reduction. The data doesn’t lie.
What If the Test Shows Low Cortisol?
If your cortisol stays below 14 mcg/dL, you’re not ready to stop. Keep taking your replacement dose. Don’t panic. This isn’t failure-it’s normal. Your adrenals are still asleep. Keep tapering slowly, and retest in 4-8 weeks. Some patients need multiple tests over months before their levels climb into the safe range.And don’t confuse adrenal insufficiency with steroid withdrawal syndrome. The latter causes anxiety, insomnia, joint pain, and mood swings-but your cortisol levels will be normal. It’s your nervous system reacting to the loss of the drug, not your adrenals failing. The fix? Slow the taper. Give your body more time to adjust.
Stress Dosing: Don’t Skip This
Even after you’ve stopped steroids, your body might still need extra cortisol during illness, injury, or surgery. That’s called stress dosing. A simple cold could send you into crisis if you’re not prepared.Every patient on long-term steroids should carry a steroid alert card. It says: "I am on or have recently stopped glucocorticoids. I need emergency hydrocortisone if I’m seriously ill or injured."
And yes-this matters even if you think you’re "off" the drugs. Recovery can take over a year. If you’re sick and your cortisol levels are still low, you need to double or triple your dose until you’re well. No exceptions.
Who’s Doing This Right?
Academic medical centers have it down. 97% of U.S. teaching hospitals have formal tapering protocols. But in community clinics? Only 63% do. And in rural areas? Many patients have to drive hours for ACTH testing. One primary care doctor on Reddit wrote: "I send patients 3 hours away. Half never show. Then they end up in the ER with adrenal crisis."That’s why the NIH is funding research into point-of-care ACTH tests-something you could get in your doctor’s office in minutes. And Epic Systems is building HPA axis tracking into electronic health records for 2025. The future is faster, smarter testing.
What Patients Say
A survey by Adrenal Insufficiency United found that 78% of patients felt anxious during tapering. 42% had severe withdrawal symptoms-headaches, shaking, nausea-even when following the rules. But those who used structured protocols with ACTH testing reported far fewer crises. One parent on the Parent Project Muscular Dystrophy site wrote: "We tried a fast taper once. My son lost muscle strength. With the Nicholoff Protocol, he stayed strong. We knew when to stop because the test told us."The Bottom Line
Stopping steroids isn’t about willpower. It’s about physiology. Your adrenals don’t respond to deadlines. They respond to time, safety, and data. ACTH stimulation testing is the only reliable way to know when your body is ready. Skipping it risks death. Following it saves lives.If you’re on long-term steroids, ask your doctor: "When will we do the ACTH test?" If they say "We’ll just watch you," push back. You deserve a plan backed by evidence-not guesswork.





9 Comments
They act like this is new info, but anyone who’s been on steroids longer than a weekend knows this is life-or-death. I almost died because my doctor said 'just cut it in half.' My adrenals didn’t care about his schedule.
Now I carry my alert card like a damn badge of survival.
Interesting how the article frames ACTH testing as the 'gold standard'-but let’s be real, most endocrinologists don’t even know how to interpret the results properly. I’ve seen labs report 17.8 as 'normal' when the cutoff is 18. That’s not precision, that’s negligence wrapped in jargon.
And don’t get me started on the 'gray zone.' It’s just a way to avoid making a decision.
Let me tell you something: if your doctor isn’t pushing ACTH testing, they’re not doing their job. I watched my sister go from 'just tapering' to flatlining in the ER because they thought 'she looked fine.'
She didn’t look fine. She was dying. And no one listened.
These aren’t guidelines-they’re lifelines. If you’re not testing, you’re gambling with someone’s life. And that’s not medicine. That’s malpractice with a stethoscope.
Just wanted to say thank you for writing this. I was terrified during my taper-felt like I was walking on glass every day.
When we finally did the ACTH test and saw my cortisol hit 19.2? I cried in the parking lot.
You’re not weak for needing time. You’re brave for sticking with it. Keep going. You’ve got this.
And yes, stress dosing matters-even when you think you’re 'off.' I learned that the hard way during a bad cold last winter.
While the article presents ACTH testing as a panacea, it conspicuously omits the fact that cortisol assays are notoriously unreliable across laboratories. The 18-20 mcg/dL threshold is derived from a single cohort study with minimal external validation. Furthermore, the Endocrine Society’s 2024 guidelines were co-authored by individuals with undisclosed ties to pharmaceutical manufacturers of cosyntropin.
One must question whether this is medicine-or a profit-driven protocol disguised as science.
Really appreciate this breakdown. I’ve seen too many people get told 'you’re fine' and then crash six months later.
My cousin went from 20mg prednisone down to zero in 3 weeks. Got hospitalized with adrenal crisis. They didn’t even test her.
She’s doing way better now-slow taper, regular tests, stress dosing on standby. It’s not glamorous, but it works.
Thanks for reminding everyone that this isn’t about willpower. It’s biology.
It is imperative to underscore the clinical significance of ACTH stimulation testing in the context of prolonged glucocorticoid administration. The physiological phenomenon of hypothalamic-pituitary-adrenal axis suppression is well-documented, yet under-recognized in primary care settings. The proposed tapering schedules, while empirically derived, must be individualized based on baseline health status, duration of therapy, and comorbid conditions. Furthermore, the integration of point-of-care diagnostics, as referenced in the NIH initiative, represents a paradigm shift toward patient-centered endocrine management. Continued advocacy for standardized protocols remains essential.
Of course the 'experts' say testing is the gold standard-because they’re the ones getting paid to run the tests. Meanwhile, real people are getting told to 'wait and see' while their bodies fall apart.
And let’s not pretend the PJ Nicholoff Protocol is some miracle. It’s just a slow taper with fancy labels. The real problem? Doctors don’t want to spend the time. So they push patients out the door with a pamphlet and a prayer.
Don’t believe the hype. This system is broken-and the only person who cares enough to fix it? You.
They’re not testing to save lives. They’re testing to keep you dependent. Look at the numbers: 97% of teaching hospitals have protocols. Coincidence? Or is this a cash cow disguised as care?
Every time you get tested, they bill it. Every time you need another round, they profit.
And don’t get me started on the 'steroid alert card'-that’s not safety. That’s a liability shield for hospitals.
They want you scared. So you keep coming back.
Wake up.