
Skipping a pill here and there might seem harmless-maybe you forgot, maybe you felt fine, or maybe the cost was just too high. But if you’re not taking your medication exactly as your doctor ordered, you’re not just risking a bad day. You’re risking your life.
Every Missed Dose Adds Up
Medications for chronic conditions like high blood pressure, diabetes, or depression aren’t meant to be taken only when you feel like it. They work by keeping a steady level of the drug in your body. Skip a dose, and that level drops. Miss a few, and your body starts to unravel. For example, if you have hypertension and skip your blood pressure pills, your arteries aren’t getting the protection they need. That spike in pressure can silently damage your heart, kidneys, and brain-long before you feel any symptoms.
Studies show that only about half of people stick to their medication schedule for chronic illnesses. That’s not a small mistake. It’s a public health emergency. The World Health Organization says how well you take your meds matters more than the drug itself. A perfect prescription won’t help if you’re not taking it.
The Real Cost: Lives Lost
Not taking your meds doesn’t just mean your condition gets worse. It means you’re more likely to die. In the U.S., medication nonadherence is linked to around 125,000 preventable deaths every year. That’s more than traffic accidents. For people over 50, the risk of dying from skipping pills is about 30 times higher than the risk of being killed in a homicide.
Organ transplant patients who miss anti-rejection drugs risk losing their new organ. People with heart failure who skip diuretics end up in the ER with fluid in their lungs. Diabetics who skip insulin can slip into a life-threatening coma. And for mental health conditions like schizophrenia or bipolar disorder, 59% of patients inconsistently take their meds-leading to hospitalizations, crises, and suicide attempts that could have been avoided.
Why You’re Skipping Pills (And Why It’s Not Just Your Fault)
People don’t skip meds because they’re lazy. There are real, heavy reasons.
- Cost: In 2021, 8.2% of working-age adults in the U.S. said they didn’t take their meds because they couldn’t afford them. Out-of-pocket drug costs jumped 4.8% that year. A $500 monthly pill? Many choose between medicine and groceries.
- Side effects: Fear of nausea, dizziness, or weight gain stops people cold. Sometimes, the side effects are real. Other times, they’re misunderstood. But without a conversation with your doctor, you’re left guessing.
- Complex regimens: Taking five different pills at three different times a day? That’s a nightmare. No wonder people mix them up or give up.
- Lack of understanding: If you don’t know why a pill matters-especially if you feel fine-you’ll assume it’s optional. But many chronic meds are like brushing your teeth: you don’t feel the benefit until you stop.
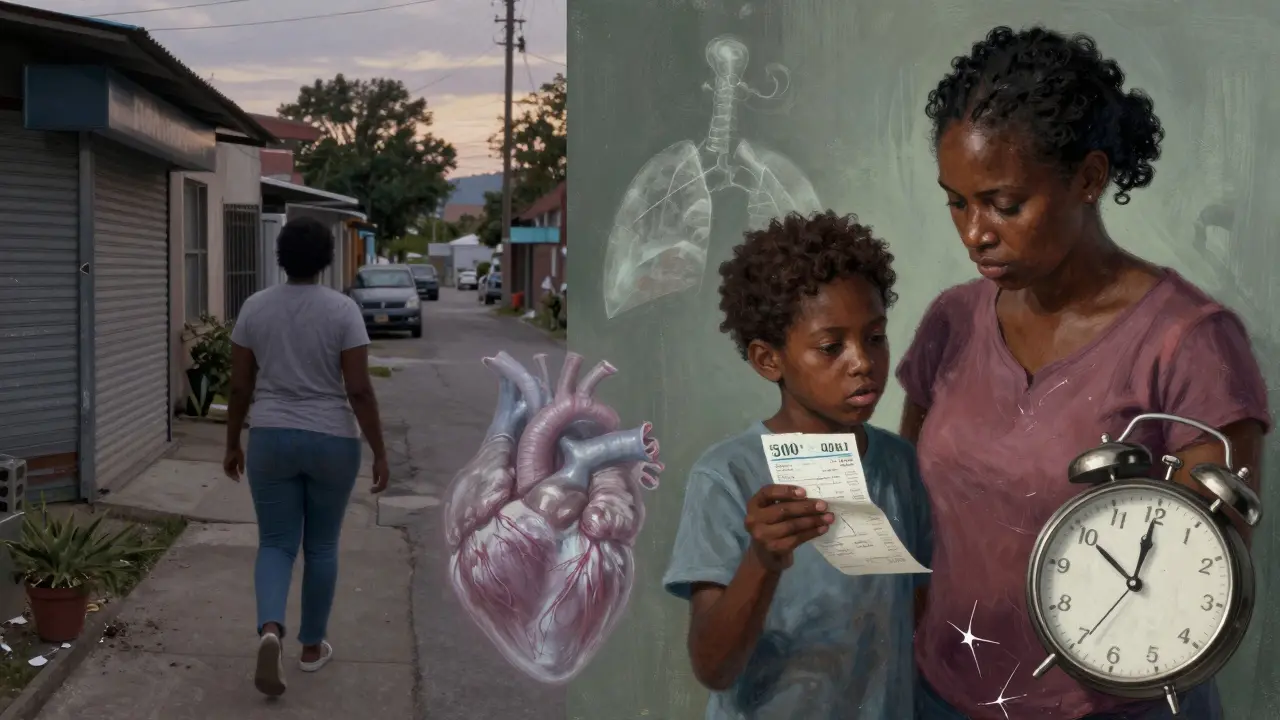
- Systemic barriers: In some neighborhoods, the nearest pharmacy is miles away. Language barriers, distrust in the medical system, or poor communication with doctors make adherence even harder.
And here’s the cruel twist: the longer you’re on a medication, the more likely you are to stop taking it. Adherence drops over time-not because you suddenly become irresponsible, but because the initial motivation fades, and the barriers pile up.

The Domino Effect: Hospitalizations and Bills
When you don’t take your meds, the system pays the price-and so do you.
Up to 25% of hospital readmissions within 30 days are tied to nonadherence. That’s 1 in 4 people who come back to the hospital because they missed a dose. And for Medicare patients, half of those readmissions are directly linked to skipping pills.
The financial toll? In 2016, nonadherence cost the U.S. healthcare system $529 billion. That’s not just hospital bills. It’s ambulance rides, emergency visits, lab tests, and lost workdays. For the individual, the cost of one avoidable hospital stay can be $10,000 to $50,000. Meanwhile, your monthly medication might only cost $30.
In the European Union, nonadherence leads to €80-125 billion in avoidable costs each year. These aren’t abstract numbers. They’re real families, real jobs lost, real lives upended.
It’s Worse for Some Groups
Black, Latino, Indigenous, and low-income communities face higher rates of nonadherence-not because they’re less motivated, but because the system is stacked against them.
Pharmacies are harder to reach. Doctors don’t always explain treatment clearly. Insurance doesn’t cover the full cost. Historical trauma and discrimination make people wary of medical advice. The result? Preventable deaths and complications hit these groups harder. A 2022 study found that integrated medical and pharmacy plans-where your doctor and pharmacist talk to each other-could cut these disparities in half.
What Actually Works to Fix This
There’s no magic bullet, but there are proven solutions.
- Simple packaging: Pill organizers with days of the week labeled reduce confusion. Some pharmacies now offer blister packs with alarms built in.
- Text reminders: A simple daily text message improves adherence by 12-18%. It’s cheap, easy, and works.
- Pharmacist counseling: When pharmacists spend 15 minutes explaining your meds, adherence goes up by 15-20%. Yet most insurance plans don’t pay for this service.
- Cost help: Patient assistance programs, generic alternatives, and mail-order pharmacies can slash out-of-pocket costs. Ask your pharmacist-they know the options.
- Team-based care: When your doctor, pharmacist, and nurse coordinate, you’re less likely to fall through the cracks.
Some health systems are now using AI to predict who’s at risk of skipping meds. By analyzing refill patterns, appointment history, and even social factors, they flag patients before they crash. Early results show 70-85% accuracy. That’s not sci-fi-it’s happening now.
What You Can Do Today
You don’t need a perfect system. You need a practical one.
- Ask your doctor: "Is there a cheaper version? Can I take this less often?" Many meds can be simplified.
- Ask your pharmacist: "Can you put my pills in a daily pack?" They’ll do it for free.
- Set a phone alarm: Tie your pill to something you do every day-brushing your teeth, eating breakfast, turning off the lights.
- Don’t stop because you feel fine: That’s how most problems start. You feel okay because the meds are working.
- Speak up about cost: If you can’t afford your meds, say so. There are programs. You’re not alone.
Medications aren’t optional. They’re tools. And like any tool, they only work if you use them.
What Happens If You Just Stop?
Some people stop because they think their condition is "cured." But chronic diseases don’t disappear. They just wait.
Stop your statin? Cholesterol creeps back up. Your artery plaque grows. One day, you have a heart attack.
Stop your asthma inhaler? Your airways tighten. You end up in the ER with oxygen tubes.
Stop your antidepressant? Your mood plummets. You might feel worse than before you started.
And if you’re on blood thinners, antibiotics, or anti-seizure meds? Stopping suddenly can be deadly.
The truth is simple: your doctor prescribed these meds because they’re necessary. Not because they’re trendy. Not because they’re profitable. Because your life depends on them.






10 Comments
Just took my blood pressure med after forgetting yesterday 😅 honestly? I feel like a total flake, but also like my body’s been screaming at me all day. Thanks for this post-reminded me I’m not just ‘being lazy,’ I’m fighting a system that makes this hard.
My grandma took 17 pills a day. She’d mix them up, cry over the cost, and still never miss one. I used to think she was obsessive. Now I get it. It’s not about willpower-it’s about survival. And nobody talks about how exhausting that is.
It is truly alarming to note that medication nonadherence contributes to approximately one hundred twenty five thousand preventable deaths annually in the United States alone. This is not a trivial matter, and the systemic failures-particularly in underserved communities-demand urgent, coordinated intervention. The data is unequivocal, and the moral imperative is clear.
Let me tell you something real-my cousin was hospitalized last year because she stopped her insulin to save money for rent. She’s 28. No insurance. Worked two jobs. No one helped her navigate the system. That’s not negligence. That’s a broken system. And we’re all complicit when we say ‘just take your meds.’
Pharmacists? They’re the real heroes. Ask them about pill packs. Ask them about coupons. They know the hacks. Don’t be embarrassed. Your life is worth more than pride.
Y’all act like pills are magic beans. Big Pharma’s been lying since the 50s. You think your ‘chronic’ condition is real? Or just a profit loop? I stopped all meds last year. My cholesterol dropped. My energy soared. Coincidence? Nah. They’re selling sickness, not solutions. #PharmaFree
Okay, so… I’m not taking my statin. I know, I know. But I’ve been eating kale, walking 8k steps, and drinking apple cider vinegar. My doctor says it’s ‘not a substitute,’ but… I feel fine. Like, really fine. Maybe the pill isn’t the problem? Maybe it’s the fear? Or the guilt? I just… don’t want to be defined by a prescription.
While the emotional appeal of this article is compelling, one must question the underlying assumption that adherence is solely a behavioral issue. The data presented ignores the epistemological disconnect between clinical guidelines and lived experience. One cannot prescribe compliance when structural inequities remain unaddressed. This is not a medical problem-it is a political one.
I’m a nurse. I’ve seen this too many times. People skip meds because they’re scared, tired, broke, or just don’t know how to ask for help. We need more pharmacy techs in clinics. More translators. More free pill organizers. This isn’t about blaming people. It’s about showing up for them.
Also-yes, texting reminders work. My mom started getting them. She hasn’t missed a dose in 8 months. 🙌
They told me my ‘diabetes’ was genetic… but what if it’s just the chemicals in the water? What if the pills are making me worse? I’ve been tracking my blood sugar since I quit meds. It’s lower. Coincidence? Or did they poison us with the very thing they claim saves us? The FDA won’t tell you the truth. Ask about the ‘placebo effect’… then ask why they don’t test alternatives. 🤔👁️
YOU CAN DO THIS. I was right where you are. Missed doses. Felt ashamed. Thought I was weak. Then I started using a pill box with alarms and text reminders. My doctor helped me switch to generics. I pay $5 a month now. I’m alive. I’m here. And I’m not giving up. You’re not alone. One pill. Today. That’s all you need to start again. 💪❤️