
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s the result of one of the most tightly controlled processes in modern medicine. The U.S. Food and Drug Administration (FDA) doesn’t just approve generic drugs because they’re cheaper. They approve them because they must meet the same exact standards for safety, quality, and strength as the original brand-name drug.
What Makes a Generic Drug the Same?
A generic drug isn’t a copy. It’s a precise replica - down to the last molecule. The FDA requires that every generic contains the same active ingredient, in the same strength, and delivered the same way as the brand-name drug. That means if your prescription is for 10 mg of lisinopril, the generic must deliver exactly 10 mg of lisinopril, not 9.5 or 10.7. It must be taken orally, just like the original. No shortcuts.
The FDA calls the original drug the Reference Listed Drug (RLD). Every generic must prove it performs identically to that RLD. This isn’t about appearance or packaging. It’s about what happens inside your body. The active ingredient must dissolve at the same rate, be absorbed into your bloodstream at the same speed, and reach the same concentration level. If it doesn’t, it doesn’t get approved.
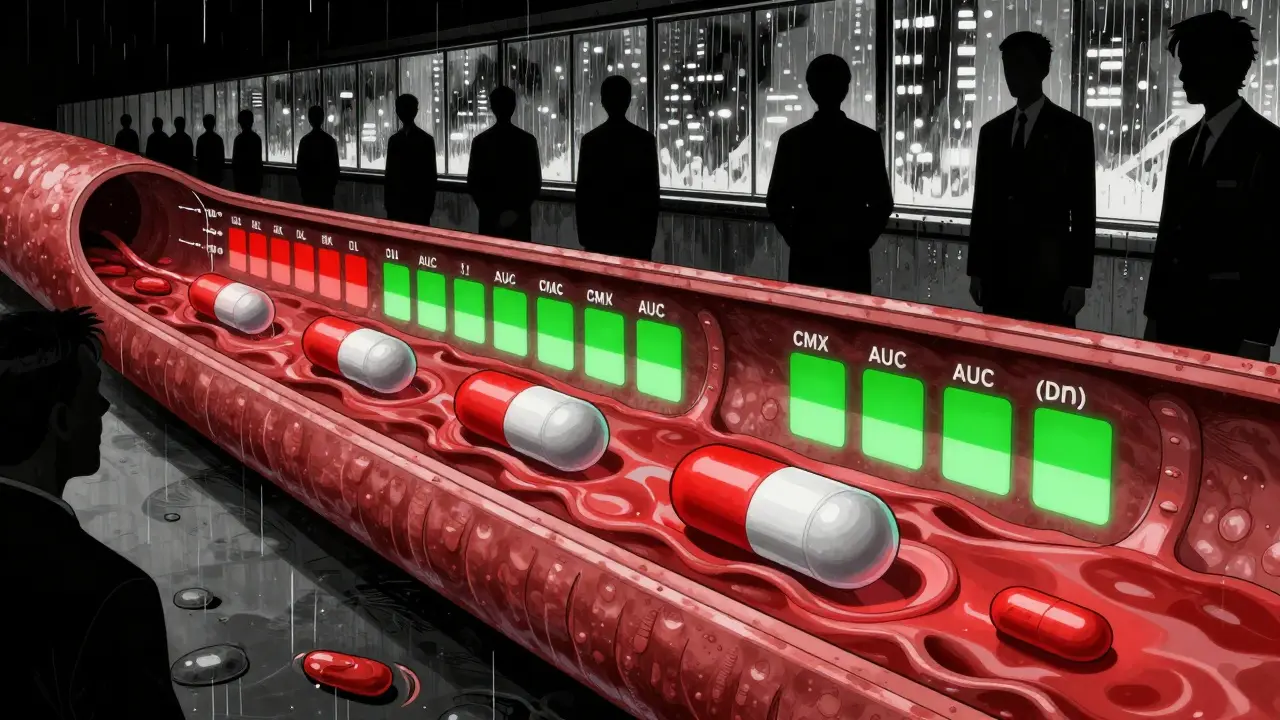
The Core Test: Bioequivalence
The most critical part of approval is bioequivalence. This isn’t a vague claim. It’s a hard science test. The FDA requires manufacturers to run studies in healthy volunteers, measuring how quickly and how much of the drug enters the bloodstream. The key numbers are Cmax (peak concentration) and AUC (total exposure over time).
For most drugs, the generic’s results must fall between 80% and 125% of the brand-name drug’s results. That’s not a wide gap - it’s a narrow window designed to ensure no meaningful difference in how the drug works. If a generic hits 79% or 126%, it’s rejected. No exceptions.
Some drugs need tighter controls. For narrow therapeutic index drugs - like warfarin, levothyroxine, or phenytoin - where even small changes can cause serious side effects, the FDA demands an even narrower range: 90% to 111%. In the case of levothyroxine, the standard is now 95% to 105%. These aren’t arbitrary numbers. They’re based on decades of clinical data showing what’s safe and effective.
Manufacturing Must Be Perfect
Even if a drug works perfectly in a lab, it won’t get approved unless it’s made the right way. Every generic manufacturer must follow Current Good Manufacturing Practices (cGMP). That means every step - from sourcing raw materials to packaging the final pill - is documented, controlled, and inspected.
The FDA doesn’t just review paperwork. They show up unannounced. In 2022 alone, they conducted over 1,200 pre-approval inspections of manufacturing sites worldwide. If a facility has even one major deficiency - like inconsistent tablet hardness, improper sterilization, or uncontrolled contamination - the application gets a Complete Response Letter. That’s a rejection. The company must fix the problem, retest, and resubmit.
One example: In 2021, Hetero Labs’ generic version of Jardiance (empagliflozin) was rejected because tablet hardness varied across batches. That’s not a minor flaw. If pills are too soft, they break in transit. Too hard, and they won’t dissolve properly in your stomach. Both scenarios mean the drug won’t work as intended.
Complex Drugs Are a Different Challenge
Not all generics are created equal. Simple pills - like metformin or atorvastatin - are relatively easy to copy. But complex products? That’s where things get hard.
Inhalers, injectables, topical creams, and extended-release tablets involve more than just chemistry. They require precise device engineering, controlled release mechanisms, and specialized delivery systems. The FDA approved only 3 out of 27 applications for generic EpiPens between 2015 and 2020. Why? Because the auto-injector mechanism had to match the original in feel, force, and timing. A 0.1-second delay could mean the difference between life and death in an allergic reaction.
Even among conventional generics, complexity matters. A 2021 analysis found that only 58% of complex generic applications were approved within three review cycles, compared to 76% for simple ones. The average approval time for complex generics is nearly 47 months - almost two years longer than for standard pills.
Why the Process Takes So Long
You might think the generic approval process is faster because it doesn’t require new clinical trials. And it is - but it’s not easy. The FDA receives fewer than 10% of generic applications that get approved on the first try. Why? Because the paperwork is overwhelming.
A typical ANDA (Abbreviated New Drug Application) runs 5,000 to 10,000 pages. It includes chemistry data, manufacturing details, stability studies, bioequivalence reports, and proposed labeling. One mistake - a missing batch record, an unclear dissolution method - can delay approval by months.
Companies that succeed early often use the FDA’s Pre-ANDA program. This lets them meet with regulators before submitting, ask questions, and fix issues ahead of time. According to a 2023 survey, 78% of successful applicants used this route. Those who didn’t? They faced longer delays and higher rejection rates.

Costs and Savings - The Real Impact
Developing a brand-name drug costs about $2.6 billion. Developing a generic? Around $1.3 million. That’s why generics make up 90% of U.S. prescriptions but only 23% of total drug spending. In 2022, they saved the healthcare system $373 billion.
But the savings aren’t just about price. They’re about access. Without generics, millions of people couldn’t afford medications for diabetes, high blood pressure, or depression. The FDA’s approval system ensures that low cost doesn’t mean low quality. It ensures that a $5 generic pill works just as well as a $50 brand-name one.
What Happens After Approval?
Approval isn’t the end. The FDA keeps watching. Once a generic hits the market, they monitor adverse events, run inspections, and test samples. If a generic starts causing unexpected side effects, or if manufacturing quality slips, the FDA can pull it from shelves.
Post-market surveillance has shown that 98.7% of generic drugs perform identically to their brand-name counterparts over 15 years of real-world use. That’s not a guess. That’s data from millions of patients.
Still, concerns linger. Some doctors worry about switching between different generic versions of the same drug - especially for patients on multiple medications. But the FDA’s position is clear: every approved generic meets the same standard. If you switch from one generic to another - both FDA-approved - you’re not switching to a different drug. You’re switching to another version of the same drug.
What’s Next?
The FDA is pushing to speed up approval of complex generics. Their goal? Get 50% of these harder-to-make drugs approved within two review cycles by 2027. Right now, only 28% make it that fast.
They’re also expanding their guidance for products like biosimilars, injectables, and nasal sprays. With over 127 complex brand-name drugs still without generic competition - worth $52 billion in annual sales - there’s a huge opportunity to bring down costs further.
But the core rule hasn’t changed since 1984: if a generic doesn’t meet the same safety, quality, and strength standards as the original, it doesn’t get approved. Period. That’s why millions of Americans trust generics. Not because they’re cheap. Because they’re proven.
Are generic drugs as safe as brand-name drugs?
Yes. Every FDA-approved generic drug must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. It must also meet the same strict standards for purity, stability, and bioequivalence. The FDA requires that generics perform identically in the body. Post-market data shows that 98.7% of generic drugs have equivalent clinical outcomes to their brand-name counterparts over 15 years of use.
How does the FDA test if a generic drug works the same way?
The FDA uses bioequivalence studies. Healthy volunteers take both the generic and brand-name drug in a controlled crossover study. Blood samples are taken over time to measure how much of the drug enters the bloodstream (Cmax) and how much is absorbed overall (AUC). For most drugs, the generic’s results must fall within 80%-125% of the brand’s. For narrow therapeutic index drugs like warfarin or levothyroxine, the range is tighter - often 90%-111% or even 95%-105%.
Why do some generic drugs get rejected by the FDA?
Most rejections happen because of manufacturing issues - not because the drug doesn’t work. Common reasons include inconsistent tablet hardness, impurities in raw materials, failed stability testing, or incomplete documentation. The FDA inspects manufacturing sites closely. If a facility can’t prove consistent quality across batches, the application is rejected. For example, Hetero Labs’ generic Jardiance was turned down in 2021 due to uneven tablet hardness across production runs.
Are complex generics harder to approve than simple ones?
Yes. Simple oral tablets like metformin or atorvastatin have high approval rates. But complex products - like inhalers, injectables, topical creams, or extended-release formulations - face much higher rejection rates. Only 58% of complex generic applications are approved within three review cycles, compared to 76% for simple ones. The FDA approved only 3 out of 27 generic EpiPen applications between 2015 and 2020 because the auto-injector mechanism had to match the original exactly.
How long does it take to get a generic drug approved?
On average, it takes 32.7 months from submission to approval. For simple generics, it’s about 28.5 months. For complex ones, it can take nearly 47 months. The FDA aims to complete its first review within 10 months for standard applications and 8 months for priority ones. But most applications aren’t approved on the first try - less than 10% are. Delays usually come from incomplete data or manufacturing issues that require fixes and resubmission.
Can I trust a generic drug if it’s made overseas?
Yes. Over half of all generic drugs sold in the U.S. are manufactured overseas, mostly in India and China. But the FDA inspects all facilities - domestic and foreign - using the same standards. In 2022, the FDA conducted over 1,200 pre-approval inspections worldwide. A drug made in India must meet the same cGMP rules as one made in New Jersey. If a facility fails inspection, the drug can’t be sold in the U.S., no matter where it’s made.






14 Comments