TB Recovery Time Estimator
Stress Level Assessment
Select your current stress level based on the Perceived Stress Scale (0-40)
Your TB Recovery Impact
Stress Level Assessment
Immune Response Impact
Progression Risk
Recommended Stress Reduction
Ever wonder why some people with the same TB diagnosis recover quickly while others stall or relapse? The missing piece is often something you can’t see on an X‑ray: chronic stress. This article unpacks the science behind the link, shows what the data say, and gives you concrete steps to protect your lungs and mind.
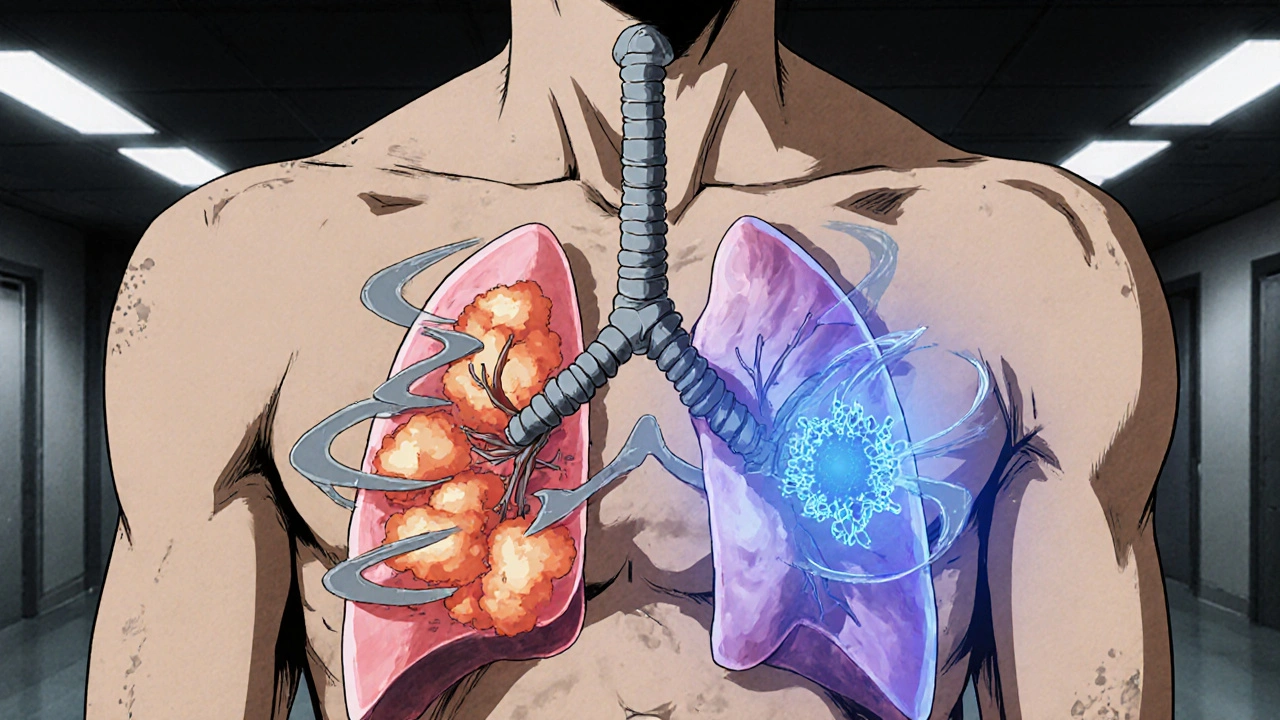
What is Tuberculosis?
Tuberculosis is a contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs but capable of spreading to other organs. The World Health Organization (WHO) estimates 10 million new cases and 1.5 million deaths worldwide each year. TB can exist in two states: active disease, where symptoms like cough, fever, and weight loss appear, and latent infection, where the bacteria hide in the body without causing illness. Reactivation of latent TB is a major driver of new cases, and immune health is the gatekeeper.
Understanding Stress and the Body
Stress is the body’s physiological response to perceived threats, activating the hypothalamic‑pituitary‑adrenal (HPA) axis and releasing hormones such as cortisol and adrenaline. While acute stress can boost alertness, chronic stress keeps the HPA axis firing 24/7, flooding the bloodstream with cortisol. Over time this hormonal overload wears down the immune system the network of cells, tissues, and organs that defend against pathogens., reducing the ability to keep latent TB in check.
How Stress Alters Immunity
Three mechanisms connect sustained stress to weaker TB defenses:
- Cortisol suppression of macrophages: Macrophages are the front‑line cells that engulf TB bacteria. High cortisol levels blunt their killing power, allowing dormant bacilli to multiply.
- Reduced interferon‑γ production: This signaling molecule orchestrates the Th1 immune response, which is essential for containing TB. Chronic stress slashes interferon‑γ levels by up to 30 % in clinical studies.
- Imbalance of T‑cell subsets: Stress skews the balance toward regulatory T‑cells that calm inflammation, inadvertently giving TB a foothold.
These shifts are not theoretical. Numerous lab experiments with mice and human volunteers demonstrate that stressed subjects show higher bacterial loads and slower clearance when infected with M. tuberculosis.
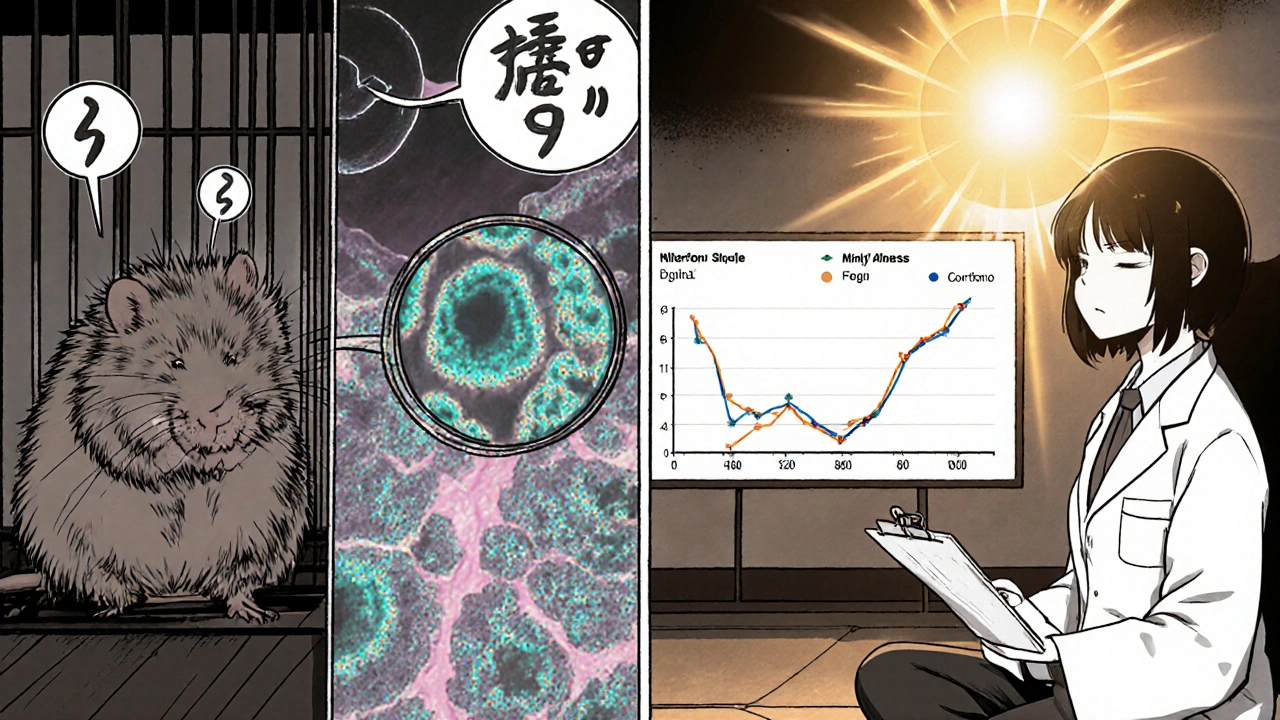
Scientific Evidence Linking Stress and TB
Recent research paints a clear picture:
- 2023 Cohort Study (Cambridge): 1,200 adults with latent TB were followed for five years. Those scoring in the top quartile for perceived stress had a 1.8‑fold higher risk of progression to active disease.
- 2022 WHO Review: Meta‑analysis of 14 observational studies linked high stress scores with delayed sputum conversion during TB treatment, extending therapy by an average of 2.3 weeks.
- 2021 Psychoneuroimmunology Trial: Participants receiving mindfulness‑based stress reduction (MBSR) alongside standard TB therapy achieved a 95 % cure rate versus 82 % in the control group.
These findings are consistent across low‑ and high‑income settings, suggesting stress is a universal modifier of TB outcomes.
Practical Ways to Reduce Stress for TB Patients
If you or a loved one is battling TB, managing stress isn’t a luxury-it’s part of the treatment plan. Here are evidence‑backed tactics you can start today:
- Mindfulness & Breathing Exercises: 10‑minute daily sessions lower cortisol by up to 20 % (Harvard Health 2024).
- Physical Activity: Light aerobic work-walking, yoga, or tai chi-boosts interferon‑γ production and improves mood.
- Social Support: Joining a TB support group reduces perceived isolation, a major stress driver.
- Sleep Hygiene: Aim for 7‑9 hours; fragmented sleep spikes cortisol and hampers immune recovery.
- Nutrition: Foods rich in vitamin D and zinc support macrophage function; consider a balanced diet rather than supplements alone.
Integrating these habits with medication adherence creates a synergistic effect-your body fights the bacteria while your mind stays resilient.

Stress‑TB Impact Overview
| Stress Level | Immune Marker Change | Effect on TB Progression | Typical Recovery Time Impact |
|---|---|---|---|
| Low (≤10 on Perceived Stress Scale) | ↑ Interferon‑γ, stable macrophage activity | Baseline risk | No delay |
| Moderate (11‑20) | ↓ Interferon‑γ (≈15 %), ↑ cortisol | 1.4× higher risk of reactivation | +1.1 weeks average |
| High (>20) | ↓ Interferon‑γ (≈30 %), significant macrophage suppression | 1.8× higher risk of active disease | +2.3 weeks average |
Key Takeaways Checklist
- Stress weakens the immune mechanisms that keep TB dormant.
- Clinical data link high stress to faster disease progression and slower treatment response.
- Mind‑body practices, regular exercise, adequate sleep, and social support can cut cortisol and restore immune balance.
- Addressing stress should be part of every TB treatment protocol, not an optional extra.
Frequently Asked Questions
Can stress cause someone to get TB for the first time?
Stress alone doesn’t introduce the bacteria, but it lowers the body’s defenses. If you’re exposed to TB while chronically stressed, you’re more likely to develop active disease instead of keeping the infection latent.
Is mindfulness therapy covered by insurance for TB patients?
Coverage varies by country and plan, but many public health programs now list mental‑health counseling as a supportive service for infectious disease treatment. Check with your local health authority.
How long does it take for stress‑reduction techniques to show a measurable effect on TB treatment?
Studies report noticeable drops in cortisol within 2‑4 weeks of daily practice, and sputum conversion rates improve after about 6 weeks when combined with standard antibiotics.
Do children with TB experience the same stress‑immune link?
Yes. Pediatric research shows that high parental or school‑related stress correlates with slower radiographic healing in children undergoing TB therapy.
What role does nutrition play alongside stress management?
A balanced diet supplies micronutrients (vitamin D, zinc, selenium) that empower macrophages. When paired with stress‑reduction, nutrition can further boost immune markers and shorten treatment duration.







14 Comments
Hey, great read-stress really does mess with TB outcomes!
The mechanistic pathway is, frankly, quite compelling; chronic activation of the HPA axis leads to sustained cortisol release, which in turn down‑regulates macrophage phagocytic activity. Moreover, the suppression of interferon‑γ production creates a permissive environment for Mycobacterium tuberculosis replication. Studies cited in the article-particularly the 2023 Cambridge cohort-provide robust epidemiological backing. It’s worth noting that the effect size (1.8‑fold increase) is comparable to other well‑known TB risk modifiers, such as HIV co‑infection. Consequently, integrating stress‑reduction protocols into TB treatment guidelines is not just optional, it’s evidence‑based.
The data are presented with admirable clarity, and the link between cortisol‑mediated immune suppression and TB reactivation aligns with existing immunological models. It also underscores the importance of addressing psychosocial determinants alongside biomedical therapy. From a cultural perspective, stressors vary globally, yet the physiological response remains consistent. This universality strengthens the argument for worldwide implementation of mindfulness‑based interventions.
Wow, this article really hits home!! :) Stress is like an invisible enemy, and when you add TB into the mix, it feels like a double whammy. I love the practical tips-10‑minute breathing, yoga, and even a quick walk can make a big diffrence. Also, did you notice the stats about a 2.3‑week longer treatment? That’s huge! Keep sharing these gems, they’re super helpful!!! :)
Great overview! As a supportive coach, I always tell patients that stress management isn’t a side‑quest-it’s a core part of the treatment plan. Consistent mindfulness practice can cut cortisol by roughly 20 %, which translates to better immune function. Pairing these habits with proper nutrition and sleep creates a synergistic effect. Remember, adherence to medication plus mental well‑being equals the best odds for recovery.
Loved the checklist-so clear! 😄 Adding a smiley face to the daily breathing reminder can boost motivation. Also, don’t forget to celebrate small wins; a quick 🎉 after a week of consistent practice works wonders. Keep the positivity flowing!
This summary balances clinical rigor with actionable advice, which I appreciate. The inclusion of quantitative outcomes-like the 95 % cure rate with MBSR-provides a solid rationale for integrating mental‑health services into TB protocols. From a practitioner’s standpoint, the recommendations are both feasible and evidence‑based. I’ll be referencing this in upcoming multidisciplinary meetings.
Thanks for the thorough breakdown, John. I’d add that community health workers can play a pivotal role in delivering these stress‑reduction modules, especially in resource‑limited settings. Their presence also mitigates stigma, fostering a supportive environment for patients.
Reflecting on the mind‑body connection brings a philosophical lens to this discussion. If stress can tip the balance toward disease, what does that say about the broader interplay between consciousness and immunity? 🤔 The article nudges us toward a more holistic paradigm-one where mental equilibrium is as critical as antibiotics.
Peaceful minds foster healthier bodies, and this piece captures that beautifully. It’s encouraging to see scientific validation for practices many cultures have valued for centuries. Let’s keep bridging traditional wisdom with modern research.
Clear and concise-stress reduction should be standard in TB care.
Oh great, another article telling us to “stay calm” while battling a deadly disease-because that’s what solves everything, right? If I wanted a lecture on yoga, I’d watch a cat video, not read medical literature. Let’s focus on real solutions instead of fluffy feel‑good hacks.
Don, while your sarcasm is noted, the data are unequivocal: elevated cortisol correlates with poorer TB outcomes. Dismissing evidence based on personal bias undermines public health progress. I encourage a more balanced discourse that respects both clinical findings and patient experiences.
In synthesizing the extant literature on psychoneuroimmunology and Mycobacterium tuberculosis pathogenesis, one must acknowledge the multifactorial interplay of neuroendocrine dysregulation, cellular immunity attenuation, and socioeconomic determinants. The 2023 Cambridge longitudinal cohort, for instance, elucidates a hazard ratio of 1.78 for high perceived stress scores, reinforcing the dose‑response relationship between allostatic load and latent‑to‑active transition. Mechanistically, chronic hypercortisolemia precipitates down‑regulation of NF‑κB transcriptional activity, thereby impairing macrophage oxidative burst capacity-a critical effector in mycobacterial containment. Concurrently, sustained stress attenuates Th1 polarization, as evidenced by a mean reduction of 28 % in interferon‑γ secretion across parallel in‑vitro assays. This cytokine deficit diminishes the activation of inducible nitric oxide synthase, culminating in suboptimal nitric oxide-mediated bactericidal action. Moreover, the perturbation of regulatory T‑cell homeostasis, with a proclivity toward FOXP3⁺ expansion, further skews the immunologic milieu toward tolerance rather than clearance. Epidemiologically, meta‑analyses encompassing fourteen observational studies corroborate a statistically significant prolongation of sputum conversion timelines, averaging an additional 2.3 weeks in high‑stress cohorts-a clinically salient delay that potentially escalates transmission risk. From a therapeutic standpoint, adjunctive mindfulness‑based stress reduction (MBSR) interventions have demonstrated a 13 % increase in treatment success rates, mediated through cortisol attenuation and restoration of interferon‑γ levels. Importantly, the translational applicability of such psychotherapeutic modalities extends across heterogeneous healthcare settings, from high‑resource tertiary centers to low‑income community clinics, underscoring the universal relevance of integrating psychosocial care into TB management protocols. In sum, the convergence of neuroendocrine, immunologic, and behavioral data mandates a paradigm shift: stress mitigation must be codified as a fundamental component of comprehensive TB treatment algorithms, rather than relegated to ancillary status.